INTRODUCTION
Chronic illnesses are defined as diseases with a prolonged duration and involve a variety of conditions, including syndromes, physical disabilities, organic failures, leading to a reduction in a person’s normal physical and mental abilities. Chronic non-communicable diseases (NCDs) include cardiovascular diseases such as hypertension, stroke, coronary heart disease (CHD), heart failure (HF), diabetes mellitus (DM), cancer, diseases of the respiratory system such as chronic obstructive pulmonary disease (COPD) and bronchial asthma, and they are the leading cause of morbidity and mortality worldwide according to the World Health Organization1,2.
According to European Union data, there are at least 90 million people, who represent the 18.5% of the total population, over the age of 65 and the majority of them in this age group have multiple chronic NCDs3. The observed exponential increase in the incidence of the aforementioned diseases, combined with the increasingly comprehensive understanding of their adverse health effects – which are preventable – have rightly aroused the interest of the world scientific community and policy makers. In order to reduce the spread of NCDs, to raise awareness and to push local governments to prioritize appropriate measures, WHO has set the reduction of early morbidity due to chronic diseases through preventive and therapeutic actions, as a goal in Agenda 2030 for sustainable development (Target 3.4)4.
The outbreak of the SARS-CoV-2 has spread rapidly to many countries. At the time of review (April 2021) more than 140 million people had been affected worldwide and over 3 million total registered deaths had been reported. By August 2022, more than 570 million people were affected and total registered deaths rose to over 6 million5. In March 2020, WHO declared the COVID-19 infection as a pandemic6. This unprecedented health crisis has shaken health systems in most countries of the world, pushing them to radical changes and adjustments in health services provision7,8, raising, as expected, important concerns, not only for the effective management of the pandemic, but also for the efficient provision of care to patients with chronic diseases9,10.
It is now widely known that NCDs, advanced age and obesity increase the morbidity and mortality in the event of COVID-19 infection3,11. Therefore, in a period of an unprecedented health crisis, such as the COVID-19 pandemic, it is essential for these patients to adhere to public health measures, to be closely monitored, to be adequately managed, and in case of deregulation to have access and arrive at healthcare facilities on time.
Due to the high prevalence of the virus, governments around the world have been called upon to take restrictive measures, such as social distancing, local and national lockdowns, quarantine and home isolation, which radically change people’s daily lives and habits. In addition, from the very first stages of the pandemic, it was suggested that the health facilities, and especially hospitals, were high transmission hotspots of the virus, resulting in an adjustment of health services provision with an emphasis on minimizing the contacts of patients with health personnel8. The former, combined with the fear and the reluctance of citizens to come to health facilities due to the increased likelihood of exposure and infection with the new coronavirus8,12,13, as well as the growing shortages of available medical staff, led various PHC services of prevention, treatment and rehabilitation to neglect14, resulting in reduced access, discontinuities and delays in healthcare15.
The concerted effort of health systems and health policy makers to reduce the extent of the unprecedented health crisis and minimize its morbidity and mortality has shifted priorities with focus on addressing the COVID-19 pandemic, and affected, as a result, both continuity and quality of chronic care, thus predisposing the care to possible negative long-term consequences16-18.
The aim of this narrative review was to investigate the impact of the COVID-19 pandemic on the management of patients with chronic diseases in PHC. More specifically, the objectives of this study were the description of the disrupted health services, the investigation of the reasons that led to the discontinuation of chronic care provision, the description of the short-term and long-term consequences, and the outline of the main adjustments adopted by health systems around the world to ensure the continuity of chronic care services in PHC.
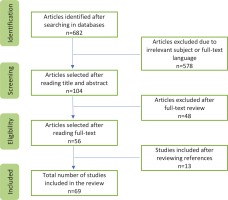
A narrative literature review of the current bibliography was conducted, in order to fill the gap in the international literature and to achieve a detailed and comprehensive composition of the limited and quite heterogeneous data of around the world19,20. The PubMed and Google Scholar databases were searched up to April 2021, using Boolean operators (AND, OR and NOT) with appropriate combinations of the following search terms: ‘chronic diseases’, ‘chronic conditions’, ‘non communicable diseases’, ‘multimorbidity’, ‘polypharmacy’, ‘primary care’, ‘outpatient care’, ‘general practice’, ‘family medicine’, ‘follow-up’, ‘management’, ‘disruption’, ‘continuity, ‘SARS-CoV-2’, ‘COVID-19’, and ‘pandemic’. Also, for the adequacy of the data, references of the articles selected for further analysis in the specific review were screened for relevant sources. Exclusion criteria from this study were articles in a language other than English and Greek, as well as studies from the gray literature.
Out of a large volume of published articles the duplicate records were initially deleted and a quick assessment of their relevance to the research questions of this study was carried out from the title, abstract and index terms. The articles, that were positively evaluated, were then read in their entirety and a short critical appraisal followed. The studies that were relevant to the topic were finally included in the present narrative review. An analysis of concepts and thematic frameworks was then performed; the relevant data of the literature were grouped and the sections of the final text of the narrative review were formulated. Collection of data, data extraction, analysis and interpretation were performed by the primary investigator. Potential disagreements were resolved by discussion among all authors until a consensus was achieved.
The search in PubMed and Google Scholar databases produced 682 articles after the deletion of duplicate records. After reviewing the titles and the abstracts, 104 articles remained. Finally, 56 articles were selected after full text reading and further 13 articles were selected from the references of the included articles. The total number of the reviewed articles was 69 (Figure 1).
DEVELOPMENTS
Since the outbreak of the pandemic, special attention has been paid by public health policy makers to preventing the spread of the SARS-CoV-2 virus (increasing the capacity for laboratory testing, contact tracing, personal protective equipment and social distance measures), as well as rapidly escalating the capacity of hospitals and their workforce to manage sudden increases in demand for care of COVID-19 cases. However, the pandemic also significantly affects many people who are not infected with the virus, especially patients with chronic diseases who faced a double threat during the first wave of the pandemic: increased vulnerability to complications and severe disease from SARS-CoV-2, in combination with the difficulties of accessing the necessary chronic care21.
We now describe the chronic care services that were neglected during the COVID-19 pandemic, the reasons why this discontinuity happened, the possible short-term and long-term consequences, and finally the adjustments of health systems to ensure comprehensive delivery of continuous and patient-centered care in times of crisis.
Chronic care services disrupted during the COVID-19 pandemic
Since the onset of the pandemic, there has been a steady shift in the balance of chronic care delivery worldwide and many regular medical visits have led to delays, postponements, rescheduling or even cancellations14, as summarized in Table 1. A survey conducted by WHO, in 155 countries, showed that patients with chronic diseases did not have access to health services related to prevention, diagnosis, treatment and rehabilitation, which posed additional barriers to the effective management of chronic diseases during the unprecedented health crisis15. In addition, a large survey conducted on health professionals from 47 countries during the first wave of the pandemic showed a large reduction or even cancellation of many scheduled health appointments, and only 14% of them continued with a physical presence, while the majority of visits were converted into distance sessions22. According to the same research, the most common chronic conditions, the care of which was disrupted during the pandemic, were: DM 38%, COPD 9%, hypertension 8%, cardiovascular diseases 7%, bronchial asthma 7%, cancer 6%, and depression 6%22.
Table 1
Chronic care services neglected during the COVID-19 pandemic
The PHC facilities around the world, in full alignment with the instructions of the WHO and the national health authorities, reorganized the provision of health services, turning it into almost monothematic and one-dimensional. Emphasis was placed on safe access and timely identification and isolation of suspected and confirmed cases of COVID-19, and as a result the provision of chronic care was largely neglected, leading many scheduled visits to postponements and cancellations23-25. A recent OECD report, which included data from many countries around the world, showed an overall decline in conventional PHC services ranging from 11% in Norway to 51% in the US21. In the United Kingdom, during the period April to August 2020, there was a decrease of 20.8% in all scheduled appointments at the PHC26 compared to the same period of 2019, while during the same time in Belgium, a country with the highest percentage of COVID-19 mortality in Europe, 25% of scheduled chronic care visits to the PHC were postponed and an appreciable number of visits were converted to digital16,27.
In US, reductions in outpatient care visits reached 70%28, while at the same time, in a study conducted during the first wave of the pandemic, there was an 81–90% reduction in regular laboratory re-examinations in two of the most common chronic diseases managed in PHC: DM and dyslipidemia. Also, a 52–60% reduction in the diagnosis and the initiation of new hypolipidemic and antidiabetic drug therapies was observed24. In Brazil, according to a large study on patients with diabetes, the postponement of regular medical PHC visits and scheduled outpatient examinations were described among the main consequences of the COVID-19 pandemic (38.4%), while 40.2% of participants stated that they had neglected and had not scheduled a medical appointment to monitor diabetes since the onset of the pandemic29.
As the priority of PHC services focused on controlling the COVID-19 pandemic, along with the management of chronic diseases, the provision of all preventive health services, including regular vaccinations, was significantly disrupted30,3. Although there are few studies examining the effects of the pandemic on the vaccination of children and adults, a recent analysis showed that in 2020, compared to 2019, vaccination rates (with the exception of influenza vaccination, which may have increased32), decreased by 60% in adults aged 19–49 years and by 83% in adults aged ≥65 years during the pandemic33. Similar data were available from many countries around the world31, confirming the worrying WHO reports of a reduction in vaccination activities worldwide during the pandemic34.
In addition to the postponements and cancellations of many scheduled PHC visits, a major disruption to the continuity of comprehensive provision of high-quality care to patients with chronic diseases during the COVID-19 pandemic was the significant reduction of referrals to specialized care. In the UK, the number of referrals from PHC to cardiology clinics decreased by up to 80%, during the period of the strict restrictive measures, while simultaneously the regular outpatient cardiologic care visits significantly decreased, with only a small number of them being replaced by digital visits8. Similar barriers to the provision of outpatient chronic care have been observed in many countries around the world including Greece, Italy, US, China and India15.
The entire landscape of cancer management in PHC, from prevention and early detection to the management of cancer in patients, was irreparably affected during the COVID-19 pandemic. Screening was severely affected and thus the identification and referral of suspected oncologic cases were greatly reduced35,36. National cancer screening programs in the UK, Australia, France, US and other countries have been suspended or delayed due to the unprecedented health crisis21,37. It is reported that in the US, at the peak of the pandemic in April 2020, the screening tests for breast, colon, prostate and lung cancer were lower by 85%, 75%, 74% and 56%, respectively, compared to the same period of 201938. Also, in a UK survey of 7500 people, almost half of the patients who experienced potential cancer symptoms (even worrying symptoms such as hemoptysis and unexplained palpable mass) avoided visiting a PHC professional39. Finally, in many countries there have been delays, rescheduling, cancellations in performing laboratory (e.g. cancer markers) and imaging examinations (e.g. CT, MRI) in chronic oncology patients36,40.
The impact of the pandemic on the treatment of acute cases was equally important. Undoubtedly, emergency departments (EDs) play a critical role in diagnosing and treating life-threatening conditions that may lead to severe disability or death, but during the pandemic their role has been significantly underestimated. Although people with chronic NCDs who show signs or symptoms of a serious illness need to seek immediate care, even during the pandemic, international empirical data reveal the opposite41.
In Italy, there was a dramatic decrease of 53% in patients who came to the ED in March 2020 and 63% in April 2020, compared to the same periods of 2019, and this decrease was with regard to emergency cases of all medical specialties and especially patients with CHD and myocardial infarction13, with the sole exception of an increase in attendance of patients with symptoms of the respiratory system (fever, cough, shortness of breath) that accompany the outbreak of the new coronavirus9. Data from US national registries showed that ED visits decreased by 42% to 50% in the first months of the pandemic compared to the pre-pandemic period21, while it is worth noting that the largest reductions were found in life-threatening acute events such as myocardial infarction (23%), stroke (20%) and hyperglycemic conditions (10%), which usually signal deregulation of chronic diseases41. According to a recent observational study from Greece, findings were quite similar, as a significant reduction in visits to the cardiology ED was observed in March (41.1%) and April (32.7%) of 2020, compared to January of the same year42.
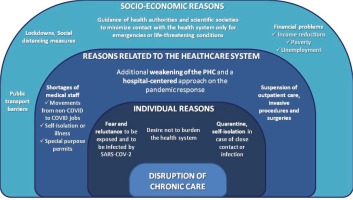
Reasons that contributed to the disruption of chronic care during the COVID-19 pandemic
There are many reasons that contributed to the disruption of chronic care during the COVID-19 pandemic (Figure 2). Perhaps the most important reason for disrupting the continuity and quality of the chronic care provided was the change in the priorities of the health systems and the concerted effort of all stakeholders to reduce the extent of the unprecedented health crisis and to minimize its morbidity and mortality16. Indeed, the managerial and financial interest of health policy makers around the globe (Governments, Ministries of Health, Public Health Organizations) has been focused on combating the emergency of the pandemic and, as a result, the effective management of chronic diseases has been marginalized8,22. The priorities changed, resource allocation was renegotiated and necessary logistical equipment (PPE, hospital and ICU beds, respirators), as well as human resources, were transferred not only from non-COVID to exclusively COVID12,13,17, but also from primary to secondary and tertiary facilities, weakening further the already weakened PHC and dismantling its essential role in the effective management of the health crisis23. Consequently, many non-emergency chronic care services have led to delays, postponements and cancellations, overturning the necessary continuity of chronic care17,18.
Since March 2020, when WHO declared the COVID-19 infection a pandemic6, local health authorities have made recommendations for staying at home and minimizing the movement of citizens, in order to slow the spread of SARS- CoV-2 and to reduce the burden on the healthcare system41. The UK government in order to raise awareness and encourage citizens to limit their social activities and contacts with the health system, organized and implemented an educational campaign with the main slogan: ‘Stay Home, Save Lives, Protect the NHS’8. A similar campaign was carried out in Greece by the National Organization of Public Health with the main message: ‘Stay Home. Stay Safe’, which indirectly prevented citizens from visiting health professionals except in urgent, life-threatening cases. In fact, global guidance on mitigation measures has placed particular emphasis on vulnerable populations, including patients with chronic NCDs3, risking comprehensive care, which requires regular interactions between patients and healthcare providers to educate patients, prescribe medication and treat potential physical or mental complications23. In the same direction and in line with national recommendations, many scientific medical societies encouraged patients with chronic diseases to stay at home and visit the healthcare system only for emergencies41,43.
As the number of cases with SASR-CoV-2 increased and the pressure on healthcare systems around the world escalated, specialists on infectious disease did not effectively respond on the increased needs of these patients, resulting in the urgent recruitment of several physicians of other specialties to assist in the management and treatment of COVID patients, without often the appropriate special training and preparation9. Consequently, during the pandemic due to the marked movements of doctors, nurses, and other healthcare professionals from non-COVID to COVID-19 jobs to support large numbers of suspected and confirmed cases, severe shortages of health personnel on chronic care were observed. In fact, special emphasis was given to the secondary and tertiary hospital facilities with simultaneous degradation of PHC12,15. In the UK, for example, in June 2020 there were 1.8% fewer GPs in the PHC compared to June 201926, with similarly worrying findings from Wuhan, China17, and Brazil, which were expected to lead to rescheduling and cancellation of many chronic care services29. In addition to the mandatory motivations of medical staff, quarantine, home isolation or even hospitalization of doctors and nurses, who were exposed to or infected with the new coronavirus, weakened further the healthcare system for non-COVID cases3,12,17,37.
One of the main reasons for the reorganization of chronic care was the reluctance and fear of the general population and especially of the patients with NCDs to come to the health facilities to seek help, due to the increased risk of exposure and infection by SARS-COV-28,11,12,16,22,28,42-45. Indeed, from the very first stages of the pandemic, health facilities, especially hospitals, became high transmission hotspots of the virus, resulting in the re-adjustment of health services with an emphasis on minimizing the interactions between patients and healthcare professionals8. Overall, it is estimated that more than 40% of US adults have delayed or avoided seeking care due to severe pandemic anxiety and fear, with 12% referring to health emergencies or life-threatening conditions46. In addition, in some cases, citizens were unable to access health facilities, either due to public transport problems or the inability to move due to the absence of relatives. In fact, the aforementioned situation was observed with increased frequency in the elderly or people with disabilities, who are more often plagued by multiple chronic comorbidities9,17.
Consequences of chronic care delays during the COVID-19 pandemic
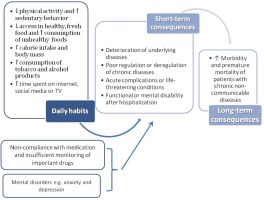
Unhealthy diet and lack of physical activity are the main modifiable risk factors responsible for chronic NCDs4. Restrictive measures such as social distancing, quarantine and lockdowns, adopted by many countries around the world to limit the spread of the new coronavirus, have had a negative effect on the daily habits of patients with chronic illnesses, adversely affecting, as a result, their management3,13,14,23. More specifically, there was a decrease in physical activity levels, a significant increase in sedentary behavior and caloric intake, an increase in the consumption of alcohol and tobacco products, and a tendency to unhealthy foods consumption14,16,23,44,47-49.
In France, a survey conducted during the first lockdown (April–May 2020) on a sample of approximately 37000 adults, found that 53% of participants reduced physical activity, 63% increased sedentary behavior, and 35% gained weight on average about 1.8 kg50. In Greece, with the exception of leisure physical activity which significantly increased, all other forms of physical activity (work, transportation and sports) decreased drastically, with an overall decrease of 16.3%51. In addition, in a large study conducted in the early stages of the pandemic, among the recommended habits for the treatment of diabetes, physical activity was most affected and decreased for 59.5% of the respondents29. The same study also found a significant increase in internet use and television watching, two habits associated with sedentary behavior, unhealthy lifestyle and consequently poor management of DM29.
Furthermore, from the early stages of the pandemic there was reduced access to safe fresh food (e.g. fruit, vegetables and fish)52 and a worrying shift towards the consumption of packaged, junk and poor quality food48. Indeed, there was an increase in calorie intake and consumption of unhealthy foods due to prolonged stay at home, increased involvement with digital media and psychological distress (anxiety, stress and insecurity)50,52. As a result, the lack of physical activity and the alarming increase in sedentary behavior of patients with chronic diseases combined with the increased body weight due to poor diet during this unprecedented health crisis may lead to long-term adverse effects not only on physical but also on mental health16,51,53.
Comprehensive care and continuous, regular clinical monitoring of patients with chronic NCDs are essential to maintain compliance with medication. The reduction in medical visits and the consequent difficult communication between patients and the healthcare team, in combination with the quarantine measures that exacerbate the already existing problems of access and universal coverage, had significant implications for medication adherence3,54. The initially conflicting emerging clinical trial results regarding the management of chronic patients infected by SARS-CoV-2, combined with often unreliable information spread by media, led to the adoption of dangerous practices by chronic patients who decided to self-manage their medication. For example, in March 2020 there were reports of a possible negative effect of angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs) (two of the most common classes of antihypertensive drugs) on the risk of infection and severity of COVID-19 infection, which led many patients to discontinue their treatment54-56. This led the European Society of Cardiology and national cardiology societies to publish clarifying guidelines about the seamless continuation of antihypertensive therapy, addressed to both physicians and patients56,57.
Due to the adoption of unhealthy daily habits, delayed seeking help and non-compliance with the recommended treatment during the pandemic, many patients with underlying diseases will experience a worsening of their condition and inevitably negative short-term health consequences13. Although it is not certain that the morbidity and mortality of patients with chronic diseases will immediately increase as a result of the systematic neglect of chronic care and postponed re-examinations, it is considered almost inevitable in the long-term that a significant number of patients who would normally have been diagnosed and treated earlier may present at the rescheduled visits – or even worse in EDs – with unregulated chronic diseases, acute complications and life-threatening conditions (e.g. myocardial infarction, stroke, hypoglycemia, diabetic foot, peripheral vascular disease)18,24,41. A large study among patients with diabetes in Brazil indicated that among the main reported effects of the COVID-19 pandemic was the elevated (59.4% of participants) blood glucose levels, as well as greater variability (31.2%) compared to the pre-pandemic period29. Similarly, the results of large multicenter retrospective observational studies from US and Korea with DM found that social distancing measures adversely affected patients’ glycemic control with a significant increase in HbA1c levels58,59. In addition, even worse were the results of observational studies conducted in Italy, US and other European countries, which indicated that mortality related to acute heart attack has almost tripled due to delayed health visits60-62.
In addition, the impact of the pandemic and measures to limit its spread on patients with chronic psychiatric disorders are significant. Indeed, reduced social interactions have led many people, especially the elderly, to loneliness and mental health disorders, such as depression and generalized anxiety disorder63. In fact, the most significant impact was on patients with pre-existing mental illness, however patients with NCDs were also greatly affected3,64. Emotional disorders, loneliness, and social isolation have been associated with poorer health outcomes, including a wide range of health indicators from increased use of health services to increased overall mortality rates65.
The real concern of the global medical community is the long-term consequences of delayed care seeking, which are not yet visible3,24 (Figure 3). Indeed, delays in the diagnosis and poor management of patients with chronic conditions during the pandemic may lead to an increase in mortality rates that are not directly related to COVID-19 infection, especially in patients with oncologic or cardiovascular diseases26,39,66,67. In fact, delayed cancer diagnoses and treatments may affect the survival rates of cancer patients21,67,68. Researchers in the UK have suggested that cancer deaths may increase by up to 20% a year after a crisis due to delayed diagnosis and treatment67,69, while a study in France concluded that delayed diagnoses could lead to excess mortality of 10–15% per month of delay70. Considering that during the COVID-19 pandemic there were several reports of excess mortality, where many of the deaths unrelated to confirmed or possible COVID-19 cases may have been attributed directly or indirectly to the pandemic, one can assume that the serious effects of the systematic neglect of chronic care have already begun to appear41.
On the other hand, social isolation and the reduction of industrial production resulted in the reduction of air pollution levels and carbon dioxide emissions during the lockdown period71,72. Previous studies have shown that even a mild, short-term improvement in air quality results in a reduction in mortality and morbidity rates in patients with chronic respiratory and cardiovascular disease73,74. Therefore, the real overall impact of the positive and (short-term and long-term) negative effects of the unprecedented health crisis on the management of patients with chronic NCDs needs to be further investigated in future studies.
At this point, it is worth noting that the effects of the pandemic are expected to be more severe in chronic patients with low socioeconomic status. For socially vulnerable groups, it has been argued that the pandemic takes on the characteristics of a syndemic that interacts and exacerbates existing NCDs and the prevailing harmful inequalities of social determinants of health75. Although during the first phases of the pandemic, COVID-19 had been characterized as a socially neutral disease75,76, which did not make discriminations and affected both the poor and the rich, a more detailed study of epidemiological data reveals that not all people are affected proportionally, but there are clear differences that reflect the already existing health inequalities which plague the world population75-79. In fact, socially vulnerable groups, ethnic minorities and other marginalized populations (such as the homeless and prisoners) are called upon to confront the new coronavirus from a different starting point80. This, combined with the fact that poorer populations are more likely to engage in unhealthy habits (e.g. smoking and alcohol consumption)81, to have underlying chronic diseases and to manifest them in a more serious form and at a younger age (which are known risk factors and predispose them to severe disease, complications and increased mortality from COVID-19 infection)76,78,81-83, to have more barriers in accessing chronic care services and to be characterized by lower level of health literacy and digital literacy, indicate the increased vulnerability of these populations to the synergistic effects of the pandemic14,46,84.
Health systems adjustments and future perspectives regarding the continuity of chronic care
Health systems around the world have tried to adapt to new and unprecedented conditions and to ensure the continuity of chronic care, the interdisciplinary nature of the PHC team and the observance of social distancing measures22,57. Although well-known for many years, the widespread implementation of telemedicine and self-monitoring have been taking place due to SARS-COV-2 induced health crisis and, at present, they may have become the main ways of managing chronic diseases in most countries of the world, widely accepted by both patients and healthcare professionals21,40.
Telemedicine facilitates the patient’s remote contact with the PHC team and it is an effective adjunct in the management of chronic diseases, as it leads to improved quality of life and reduced morbidity and mortality in chronic patients85,86. Indeed, a variety of daily medical practices, such as diagnostic, treatment and rehabilitation services, follow-up, electronic medication prescriptions, interpretation of laboratory and imaging tests, psychological support sessions, information and awareness-raising activities can take place using telemedicine (e.g. by telephone or video) in non-emergency situations9,14,17,53,87. According to the CDC, in the US, in the first quarter of 2020, the number of tele-visits increased by 50%, compared to the same period in 2019, while it is worth noting that most appointments came from patients seeking treatment for non-COVID-19 diseases45.
This increase in telemedicine use is estimated to have offset about two-thirds of the total volume of neglected chronic care visits during the COVID-19 pandemic88. The significant decrease in total visits, despite the simultaneous increase in remote sessions, indicates the wide scope of deferred care during the first months of the COVID-19 pandemic89. Although some deferred care represents outpatient care that could be postponed without immediate risk, these results also support concerns that chronic illness management may be seriously delayed88.
Self-monitoring was another practice, which gained significant ground during the COVID-19 pandemic in the management of chronic diseases in PHC87. Indeed, it has been shown that regular measurement of blood pressure and close monitoring of other modifiable risk factors (smoking, diet, exercise) at home by patients, provided that they have first procured the appropriate equipment and have been trained in its proper use, in combination with the parallel distance counseling by members of the interdisciplinary PHC team, can lead to the proper regulation of chronic diseases, early diagnosis of complications and increased compliance with medication87,90,91. Similar practices have been adopted for other chronic diseases such as continuous monitoring of blood glucose levels for patients with DM58,87,92,93 and empowerment of patients with HF8.
Finally, in order to limit the frequent visits of chronic patients to healthcare facilities and focusing on the safety of both patients and healthcare staff, an intensive and targeted effort was made to use intangible electronic medication prescription and even repeated for long periods of time, during the strict restrictive measures16,52,53,94. The innovations introduced to address the COVID-19 pandemic need to be maintained and integrated into conventional practices so that health systems are more resilient to future public health emergencies and are able to meet the challenges of aging societies and the growing burden of chronic diseases so as to improve the quality of services provided.
In fact, the COVID-19 pandemic demonstrates more than ever the importance of placing PHC at the core of health systems, both in managing the unexpected increase in demand and in maintaining continuity of care for all. Strengthening health services so that they are better equipped (both material and human resources) to prevent, diagnose and manage NCDs in the future and under any circumstances is a guarantee of success21. A strong PHC – organized in interdisciplinary teams and with innovative roles for health professionals, integrated with sustainable community health services, equipped with digital technology and well-designed work incentives – helps a successful response of health systems to be achieved14,17,26,95. Especially in the post-COVID era, PHC can be the pillar of organization and reconstruction of the ailing health system, to meet the increased health needs of the population9,12.
It is worth mentioning the significant contribution of medical students in times of health crisis. It is their deep conviction that they have already developed a solid basic knowledge and thus they are more prepared and helpful than any other group of volunteers that could be trained to support PHC professionals96. Besides, from the early stages of the pandemic, despite the global instability and the disruption of medical education, the desire of medical students to make a practical contribution to the pandemic response (including NCDs management) was remarkable97, although further research is needed in the field to determine the exact role they can play in terms of safety (both their own and that of patients)98.
Strengths and limitations
To the best of our knowledge, the present study is the first attempt to analyze the diverse direct and indirect effects of the COVID-19 pandemic on the management of patients with chronic diseases in PHC, and this is a strength of the study. However, there are some limitations to be mentioned. First, the narrative aspect of this review is a limitation. The data used were drawn from heterogeneous registries, mostly retrospective observational studies, which differed considerably in design, methodology and endpoints, while some data used came from lower-on-the-pyramid hierarchy types of studies (editorials, viewpoints, commentaries). This heterogeneity of the data as well as the overwhelming volume of peer reviewed literature due to COVID-19 make a systematic review very difficult to perform99. Second, the inclusion of articles written only in Greek and English, the exclusion of gray literature sources and preprints archives and the search in only two databases may have limited the range of data examined and analyzed in this narrative review.
CONCLUSION
From the very first stages of the COVID-19 pandemic outbreak, patients with chronic NCDs diseases were faced with a dual threat: increased vulnerability to complications and severe COVID-19 infection, combined with emerging access barriers in the necessary chronic care. In order to limit the spread of the new coronavirus, health policymakers’ priorities were modified, resource management was renegotiated, health service delivery was reorganized and the continuity and quality of chronic care was shaken, causing several problems in the effective monitoring and management of chronic diseases in the PHC.
Postponements of scheduled medical visits, delayed seeking of help and lack of medication adherence could lead to deregulation of chronic diseases, posing a risk for catastrophic health consequences in the long-term. Thus, it is very important the care of people living with a NCD to be included in the national COVID-19 response and preparedness plans, as an interconnected and closely intertwined aspect of public health in the current unprecedented conditions. To address these challenges effectively, policy cannot simply focus (administratively and financially) on the ‘virus in the hospital’. An integrated strategy is needed to address all the physical, mental and social health needs of the population who directly or indirectly are affected by COVID-19 pandemic, so that health systems will not be transformed into systems for only one disease.
Finally, in order for health systems to be resilient to health crises of this magnitude, strong and empowered primary and community health care is essential100. PHC should be the fundamental pillar of chronic care, both during and after the acute phase of a health crisis, to ensure that continuous, comprehensive and patient-centered care is maintained for all and that other levels of healthcare delivery are expedited.