INTRODUCTION
There are many infections that can be transmitted from a mother to a child. These infections of the newborn are mainly acquired during in utero (congenital) through trans-placental or ascending infection: during delivery (intra-partum) by contact with infected genital secretions, blood, and by faeces, during delivery; and during the neonatal period (postpartum) through breastfeeding, blood transfusion, and nosocomial. These infections are usually associated with some complication that becomes evident either from the maternal or fetal side, during pregnancy, after delivery, or at a later stage1. Toxoplasma gondii, others (HIV, syphilis, and measles), rubella, cytomegalovirus and herpes simplex virus 1 and/or 2 are a group of infectious diseases that are known as TORCH. These preventable infectious diseases are a public health problem because they cause maternal and neonatal morbidity, disability, and mortality. TORCH can adversely affect a pregnant woman and her fetus. The newborns of pregnant women who are infected with these diseases may have birth defects. Infections that are caused by TORCH are the major causes of bad obstetric history (BOH)2.
If a pregnant woman is infected in the first trimester, the risks are severe. The general symptoms of the disease include: premature birth, neurological abnormalities, growth retardation, damage to the eyes, liver, heart and ear, also bone lesions, hydrocephaly, nanocephaly, seizer and psychomotor retardation. Pregnancy is a normal process in human beings, despite its termination before certain months particularly before 21 gestational weeks, which is considered as an abortion and attributed to a number of factors that interrupt the pregnancy’s continuity in human reproduction1,2.
The interruption and discontinuity of pregnancy can happen due to many factors that include genetic, uterine abnormalities, endocrine and immunological dysfunctions, infectious agents, environmental pollutants, psychogenetic factors, and endometriosis. Infections that are caused by Toxoplasma gondii, rubella, cytomegalovirus and herpes simplex are major causes of pregnancy loss in humans.
During pregnancy, if any woman is infected with the above, the risk of a child born with serious birth defects and/or illness, miscarriage or stillbirth increases proportionally. A study that was conducted on abortion cases looking at the influence of TORCH infections in a first trimester miscarriage revealed a prevalence of 50.7%, 11.3%, 28.2% and 59.2% for T. gondii, rubella, CMV and HSV 1 and 2, respectively. Another hospital-based study on pregnant women who were attending antenatal clinic during their first trimester at Maternity and Children’s Hospital in Makkah, Saudi Arabia, also indicated a prevalence of 35.6% with Toxoplasma IgG antibodies, 92.1% with CMV, 93.3% with rubella, 90.9% with HSV 1, 27.1% with HSV 2, 74.4% with VZV and 0% for HIV 1 & 2 antibodies3. Another prospective study that was conducted in 64 pregnant mothers in India also documented a prevalence of 26.56%, 76.56%, 85.93% and 53.12% for seropositivity of IgG for Toxoplasma, rubella, CMV and HSV, respectively4. A study on TORCH profile in patients with bad obstetric history in India also showed a prevalence of Immunoglobulin G antibodies of 20.93%, 29.06%, 23.25% and 18.60% for Toxoplasma, rubella, CMV and HSV-2, respectively5. Therefore, the present study was conducted to assess the magnitude of the prevalence of TORCH in women who had an abortion or stillbirth, to assist in managing the problem.
METHODS
A laboratory-based cross-sectional study on the frequency and associated risk factors for the prevalence of TORCH was conducted from 28 September to 30 November 2018. The study included 44 women aged 18-45 years who were admitted at OMNRTH, in Asmara, Eritrea, due to spontaneous abortion or stillbirth, whereas women with induced abortion (therapeutic/criminal abortions) and other diseases (HIV, syphilis, and measles) were excluded. The study obtained permission and an approval from the MOH ethical and research committee, and Orotta National Referral Maternity Teaching Hospital, and consent was obtained from women with spontaneous abortion or stillbirth.
From each woman, 3 mL of venous blood was collected in a container with aseptic technique. IgG antibodies against Toxoplasma gondii, rubella, cytomegalovirus and herpes simplex were detected by IgG Combo Rapid Test Cassette (Serum), which is a rapid chromatographic immunoassay that is used for the qualitative detection of these antibodies, demonstrating an overall accuracy of 97.8% for Toxoplasma gondii, 99.2% for rubella, 99.0% for CMV and 99.2% for HSV 1 and 2. The collected data were analyzed descriptively and for any associations by χ2 test using SPSS version 25 software.
RESULTS
Sociodemographic characteristics
The study participants had a mean age of 29.3 years (SD=5.6). The majority (86%) of the mothers were married and were of Christian Orthodox religion (84%). Almost 91% were of Tigrigna ethnic group. Almost all the mothers (97.7%) who participated in the study, except one (2.3%), were non-smokers and had no smoking history (Table 1).
Table 1
Sociodemographic characteristics of the study participants, Eritrea (N=44)
| Variable | n | % |
|---|---|---|
| Age (years) | ||
| <20 | 1 | 2.3 |
| 20–24 | 10 | 22.7 |
| 25–29 | 10 | 22.7 |
| 30–34 | 14 | 31.85 |
| 35–39 | 9 | 20.5 |
| Marital status | ||
| Married | 38 | 86.3 |
| Living together | 1 | 2.3 |
| Divorced | 1 | 2.3 |
| Single | 4 | 9.1 |
| Religion | ||
| Orthodox | 37 | 84.1 |
| Catholic | 3 | 6.8 |
| Protestant | 1 | 2.3 |
| Muslim | 3 | 6.8 |
| Ethnic group | ||
| Tigrigna | 40 | 90.9 |
| Tigre | 3 | 6.8 |
| Saho | 1 | 2.3 |
| Educational level | ||
| Primary school | 8 | 18.2 |
| Junior school | 12 | 27.3 |
| Secondary school | 20 | 45.4 |
| College and above | 4 | 9.1 |
| Participants’ occupation | ||
| Housewife | 29 | 65.9 |
| Civil servant | 4 | 9.1 |
| Military/National service | 1 | 2.3 |
| Government employee | 2 | 4.5 |
| Trader or merchant | 2 | 4.5 |
| Self-employed | 2 | 4.5 |
| Commercial sex worker | 1 | 2.3 |
| Other | 3 | 6.8 |
| Partners' occupation | ||
| Farmer | 1 | 2.3 |
| Military/National service | 15 | 34.1 |
| Government employee | 9 | 20.4 |
| Trader or merchant | 5 | 11.4 |
| Self-employed | 7 | 15.9 |
| Unemployed | 1 | 2.3 |
| Other | 6 | 13.6 |
| Monthly income (Nkf)* | ||
| ≤500 | 5 | 11.4 |
| 501–1000 | 16 | 36.4 |
| 1001–1500 | 6 | 13.6 |
| 1501–2500 | 8 | 18.2 |
| >2500 | 9 | 20.4 |
| Smoking in the past year | ||
| Yes | 1 | 2.3 |
| No | 43 | 97.7 |
| Currently smoking or use of tobacco | ||
| Yes | 1 | 2.3 |
| No | 43 | 97.7 |
Obstetric history of the study participants
All study participants had no history of ectopic pregnancy. The majority of the mothers had a previous history of miscarriage or abortion, and 41%, 18%, 7% and 2% had experienced a miscarriage or abortion one time, two, three or four times, respectively. Of the mothers, 97.7% had no history of multiple gestations (Table 2).
Table 2
Obstetric history of the study participants, Eritrea (N=44)
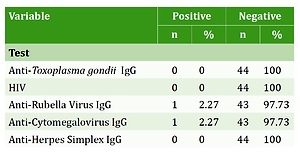
Serological test
All of the 44 mothers with pregnancy loss, who were tested for the four IgG antibodies, were found to have 0% IgG seropositivity for Toxoplasma gondii, HIV and herpes simplex. In this study only two mothers were found to be IgG seropositive; one for rubella virus and another for cytomegalovirus (Table 3).
Diagnosis or pregnancy outcome
In all, 43% (n=19) of the mothers had a complete abortion, whereas the remaining 29.5% (n=13), 18.2% (n=8), 4.6% (n=2) and 4.6% (n=2), were diagnosed as cases of incomplete abortion, missed abortion, threatened abortion and stillbirth (one preterm and one full-term), respectively. The study findings showed no significant association between age and the current miscarriage/abortion (Table 4).
Table 4
Association between age and previous/current miscarriage or abortion
| Variable | Yes | No | p* |
|---|---|---|---|
| n (%) | n (%) | ||
| Age (years) | |||
| <30 | 12 (57.1) | 9 (42.9) | 0.133 |
| >30 | 18 (78.3) | 5 (21.7) | |
| Total | 30 (68.2) | 14 (31.8) | |
DISCUSSION
The study included 44 mothers who were admitted at Orotta maternity national referral and teaching hospital. The mothers who participated in the study had different obstetric histories of pregnancies from primigravida to a multigravida of seven. In our study, the incidence of miscarriage was found to be: 2.3% for those aged <20 years; 22.7% aged 20-24 years; 22.7% aged 25-29 years; 31.85% aged 30-34 years; and 20.5% aged 35-39 years. These results are similar to those of a study6 that reported the following incidences of miscarriage: 14.81% for 15-19 years; 49.38% for 20-24 years; 24.69% for 25-29 years, and 11.1% for 30-34 years6.
Toxoplasma gondii, HIV, rubella, cytomegalovirus and herpes simplex are the known causes of infections for a fetus and loss/termination of pregnancy. In Eritrea, no study to date has evaluated the seroprevalence of TORCH in women with spontaneous abortion or stillbirth. This study indicates a very low prevalence of Toxoplasma gondii, HIV, rubella, cytomegalovirus and herpes simplex IgG antibodies in women who had a miscarriage of a recent pregnancy (complete, incomplete, missed and/or threatening abortion) or stillbirth (pre-term or full-term). All of the 44 mothers with pregnancy loss, who were tested for the four IgG antibodies, were found to have a 0% IgG seropositivity for Toxoplasma gondii, HIV and herpes simplex. In our study, only two mothers were found to be IgG seropositive; one for rubella and another for cytomegalovirus. The present study results are similar to those of studies in India, Turkey and Iraq, but the IgG seropositivity is found to be lower compared to the other studies7-10. These lower results may be attributed to the life style of Eritrean women, like consumption of properly heated and cooked food, and less contact with domestic animals. We found the prevalence of TORCH IgG to be much lower compared to the results of studies that were conducted in Saudi Arabia, India and Turkey3-6,11,12.
While the study was performed on a small sample size, the unique population and setting provide an interesting insight into TORCH in Eritrea. Despite the above, we recommend a countrywide survey among pregnant women who attend ANC during pregnancy.