INTRODUCTION
Worldwide, one in ten deaths is caused by tobacco. During the last century, the number of people dying from tobacco was approximately 100 million, this is expected to rise to one billion deaths during the 21st century1. The driving force behind the tobacco epidemic is the trans-national tobacco industry. India is the third largest producer of tobacco in the world. Andhra Pradesh is first in tobacco production with an average yield of around 193.26 million kg per year, of which 154.07 million kg are exported2.
The occupation in which people engage and its related conditions have long been known to influence oral health and in turn the overall health and wellbeing of individuals3. The reason for poor oral health in many occupations can be attributed to the work environment. Previous research has found a strong association between oral diseases and physical/psychological afflictions arising from the workload and other factors related to the workplace4,5.
Like cigarette smoking and other forms of tobacco use, working in the tobacco industry also leads to the intake of many hazardous compounds and their metabolites. These hazardous substances may react with organic molecules and lead to the formation of reactive oxygen species (ROS) that give rise to oxidative stress within the human body. Apart from causing illness and premature death, tobacco production results in other negative consequences such as economic loss for countries, poverty for individuals, deforestation and other environmental problems in countries growing tobacco6.
Oral diseases are a significant public health burden worldwide but often are given inadequate attention in many low- and middle-income countries, especially in India7. Oral diseases affect people’s everyday lives subtly but pervasively, disrupting eating, sleep, work and social roles. Oral health is essential to overall health, well-being and quality of life8. Review of existing literature has shown that oral health status and related quality of life of tobacco factory workers are not adequately documented. Since, Guntur city, the administrative capital of Guntur district, is acclaimed for its export industries, which include tobacco factories and cotton ginning mills, the workers of cotton ginning mills were considered as a suitable comparison group.
While tobacco factory workers have ready access to tobacco and are exposed to it on a daily basis at their workplace, the cotton ginning mill workers are strictly prohibited from using smoking tobacco products within the factory premises. It can be contemplated that the varying environment that exists in their workplace can affect their oral health status and thus oral health quality of life in the long-term. Hence, the main objective of the present study was to test the hypothesis that oral health status and related quality of life among the workers in tobacco factories are poorer compared to workers in cotton ginning mills.
METHODS
This cross-sectional study was carried out among workers of cotton ginning mills and tobacco factories in Guntur city, Andhra Pradesh, India. A detailed protocol explaining the nature and purpose of the study was submitted to the Institutional Review Board, and after its scrutiny, ethical clearance was obtained (MADC/IRB-IX/2016/185). The list of tobacco factories and cotton ginning mills located in Guntur city was collected from the State Tobacco Board and Cotton Ginning Mill Association of Guntur district, respectively. The nature and purpose of the study were explained to the administrators of the selected factories. Permission was then obtained to conduct the study in their premises among their factory workers. Informed consent was obtained from the study subjects (Supplementary file).
We used a specially designed proforma to collect data on demographic details, a questionnaire regarding information on work environment, adverse habits, oral health status and related quality of life. Demographic details included age, gender, education and occupation. The questionnaire (Supplementary file) consisted of ten open-ended questions on factors related to work and adverse habits. Data such as average working hours per day (item 2), use of protective wear during work (item 3), frequency of smoking per week (item 5), frequency of chewing tobacco per week (item 7), previous history of attempting to quit the use of tobacco products (item 9), awareness regarding ill effects of tobacco use (item 8) and their perception of working place as a barrier to quit tobacco use (item 10) were recorded.
We used questionnaire on Oral Health Impact Profile-14 (OHIP-14) to assess the oral health-related quality of life9. The responses were coded as ‘never’ (0), ‘hardly’ (1), ‘occasionally’ (2), ‘fairly often’ (3), and ‘very often’ (4). The total OHIP-14 score was calculated by summing responses to all 14 items, with possible scores ranging from 0 to 56; wherein the higher the OHIP-14 score, the poorer the oral health quality of life. Additionally, the answers to each question of OHIP-14 were dichotomized, and the presence of impact was defined by the answers ‘fairly often’ and ‘very often’, and for those without impact, by the answers ‘occasionally’, ‘hardly’ and ‘never’. In order to achieve culturally acceptable and conceptually equivalent OHIP-14, specific guidelines for cross-cultural adaptation were followed. The English version of OHIP-14 was translated to Telugu by two independent translators. A single translated version was developed with consensus from both translators, which was then back-translated into English by two independent translators. An expert committee consisting of all the translators and a public health dentist was then formed to develop the final version of Telugu OHIP-14. The responses for the Telugu OHIP-14 were similar to that of the English version. Face-to-face interviews with the translated version were conducted among 40 outpatients to assess the content validity of the translated questionnaire.
Test-retest reliability was evaluated using the Intra-class Correlation Coefficient (ICC). The percentage variation in response was calculated to determine whether a change in scores had occurred during the retest period. An acceptable ICC score of 0.82 was obtained for the questionnaire on OHIP-14.
Subjects were seated comfortably on an ordinary chair and examined in their respective workplace under natural light and positioned so as to receive maximum illumination. ADA type III examination technique was used wherein oral examinations were conducted using a plane mouth mirror and a WHO probe. Dentition status by tooth surface, gingival bleeding, pockets, loss of attachment, enamel fluorosis severity, dental erosion, dental trauma, oral mucosal lesions, denture status and intervention urgency were recorded using the WHO Oral Health Assessment Form 2013 by a single well-trained examiner10. Following the training session, the WHO form was recorded for the same group of randomly selected twenty-five hospital employees on successive days. The intra-examiner reliability was assessed using Cronbach’s alpha and found to be between 0.85–0.93 for various clinical parameters.
A pilot study was then carried out among randomly selected fifty tobacco factory workers and fifty cotton mill workers, to assess the feasibility of the study and to estimate the sample size for the main study. The sample size for the main study was calculated using sampling software (G power version 3.1.9.2, Heinrich–Heine–Universitat, Dusseldorf, Germany) based on the difference in the overall scores of Oral Health Impact Profile-14 between tobacco factory workers and cotton ginning mill workers. The final sample for the study was calculated to be 320 (effect size=0.4398850, α=5%, power=95%) with 160 in each group and a simple random sampling methodology was used to recruit the required number of study subjects.
The collected data were analysed using the Statistical Package for Social Sciences (SPSS) version 20.0. Descriptive statistics such as frequency, percentage, mean and standard deviation were calculated. The quantitative variables were assessed for normality using Shapiro-Wilk test, and the data were found to be normal (p>0.05). Intergroup analysis for parametric data was carried out using independent sample t-test. The qualitative data in the present study were assessed for statistical significance using Pearson’s chisquared test. Correlation between DMFT score, periodontal pocket depth, loss of attachment and OHIP-14 were carried out using Spearman’s rank order correlation coefficient test. A p<0.05 was considered as statistically significant.
RESULTS
The distribution of the workers based on demographic factors in the two study groups is compared and presented in Table 1. The distribution of workers based on the factors related to their own working environment and adverse habits is presented in Table 2. There were no statistically significant differences in the distribution of study subjects between the two groups based on age group, gender, duration of employment, use of smoking form of tobacco and with respect to the use of protective mask (p>0.05).
Table 1
Distribution of workers based on demographic factors in the two study groups
| Demographic variable | Tobacco factory workers n (%) | Cotton ginning mill workers n (%) | pa |
|---|---|---|---|
| Gender | |||
| Male | 82 (51.2) | 81 (50.6) | 0.91b |
| Female | 78 (48.8) | 79 (49.4) | |
| Age group (years) | |||
| 25–35 | 47 (29.3) | 48 (30.0) | 0.99b |
| 36–45 | 54 (33.8) | 54 (33.8) | |
| 46–55 | 59 (36.9) | 58 (36.2) | |
Table 2
Distribution of workers based on factors related to working environment and adverse habits
| Factors related to work and tobacco habits | Tobacco factory workers n (%) | Cotton ginning mill workers n (%) | pa |
|---|---|---|---|
| Years of employment | |||
| 1–5 | 38 (23.8) | 28 (17.5) | 0.38b |
| 6–10 | 56 (35.0) | 60 (37.5) | |
| >10 | 66 (41.2) | 72 (45.0) | |
| Working hours per day | |||
| <8 | 20 (12.5) | 0 (0) | <0.001c |
| 8–10 | 97 (60.6) | 137 (85.6) | |
| >10 | 43 (26.9) | 23 (14.4) | |
| Use of mask | |||
| Yes | 3 (1.9) | 4 (2.5) | 0.702b |
| No | 157 (98.1) | 156 (97.5) | |
| Smoking habit | |||
| Yes | 41 (25.6) | 36 (22.5) | 0.60b |
| No | 119 (74.4) | 124 (77.5) | |
| Frequency of smoking tobacco | |||
| More than 4 times per week | 38 (92.7) | 27 (75) | 0.066b |
| Irregularly | 3 (7.3) | 9 (25) | |
| Tobacco chewing habit | |||
| Yes | 61 (38.1) | 24 (15) | <0.001c |
| No | 99 (61.9) | 136 (85) | |
| Frequency of chewing tobacco | |||
| More than twice a week | 1 (1.6) | 2 (8.4) | <0.001c |
| More than 4 times a week | 58 (95.1) | 7 (29.1) | |
| Irregularly | 2 (3.3) | 15 (62.5) | |
| Awareness on ill effects of tobacco | |||
| Yes | 150 (93.8) | 160 (100) | 0.002c |
| No | 10 (6.2) | 0 (0) | |
| Attempted to quit tobacco | |||
| Yes | 67 (89.3) | 66 (97.1) | 0.101b |
| No | 8 (10.7) | 2 (2.9) | |
| Felt working environment as barrier to quit habit | |||
| Yes | 56 (74.7) | 7 (10.3) | <0.001c |
| No | 19 (25.3) | 61 (89.7) | |
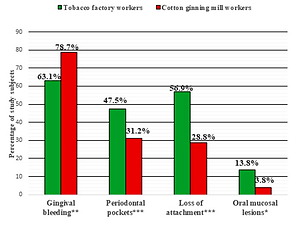
The variables of oral health status among the workers in the two groups are compared and presented in Figure 1. No statistically significant differences were noted in the mean DMFT, mean DMFS and type of traumatic dental injuries between the two groups (p>0.05). The mean overall OHIP-14 score was significantly higher among tobacco factory workers (20.81±11.59) compared to cotton ginning mill workers (16.29±9.67). The frequency of impact for each OHIP-14 domain between the workers in two groups is given in Table 3. All OHIP-14 domains were found to have a statistically significant positive correlation with DMFT, DMFS, periodontal pocket and loss of attachment in both tobacco factory and cotton ginning mill workers (Tables 4 and 5).
Table 3
Comparison of frequency of impact for each OHIP-14 domain between the workers in two groups
| OHIP-14 Domains | Frequency of impact among tobacco factory workers n (%) | Frequency of impact among cotton ginning mill workers n (%) | pa |
|---|---|---|---|
| Functional limitation | 9 (5.62) | 1 (0.62) | 0.010b |
| Physical pain | 26 (16.25) | 13 (8.12) | 0.026b |
| Psychological discomfort | 16 (10) | 25 (15.62) | 0.132c |
| Physical disability | 19 (11.87) | 31 (19.37) | 0.065c |
| Psychological disability | 17 (10.62) | 33 (20.62) | 0.014b |
| Social disability | 18 (11.25) | 4 (2.5) | 0.002b |
| Handicap | 19 (11.87) | 5 (3.12) | 0.003b |
Table 4
Spearman’s correlation coefficients between the variables of oral health status and OHIP-14 among tobacco factory workers
Table 5
Spearman’s correlation coefficients between the variables of oral health status and OHIP-14 among cotton ginning mill workers
DISCUSSION
This study focused on the oral health status and oral health-related quality of life of tobacco factory workers and compared these with those of cotton ginning mill workers.
The findings of the present study could not be compared with earlier studies as there is a paucity of literature on the oral health status of these populations. Hence, the findings of the present study have been compared with workers in other industries and general population.
The analysis of the demographic characteristics of the studied population revealed that females were equally employed in both factories as males. The reason for this could be the flexible working hours, giving women the opportunity to combine work with domestic responsibilities. Since the tobacco and cotton ginning industries are labour intensive and the monopoly demanded centralization to avoid fraud, a female workforce might be preferred11.
Tobacco use is one of the most important preventable causes of disease and death, globally. Even though the prevalence of tobacco use is declining in many countries, disparities among occupational groups still exist12. In the present study, the prevalence of smokeless tobacco use among tobacco factory workers was 38.1%, which is significantly higher than 15% for cotton ginning mill workers. An explanation for this difference could be the easy access to smokeless tobacco among tobacco factory workers on a daily basis at their workplace. Previous research conducted by Kawatra et al.13 reported a prevalence of 45.97% tobacco chewers among tobacco industry workers in Maharashtra.
Among the workers using tobacco, the proportion of the workers who perceived the working environment as a barrier to quit their habits was found to be significantly higher among tobacco factory workers (74.7%) compared to cotton ginning mill workers (10.3%). This observation supports the fact that the motivation and skills to quit tobacco habits cannot be effective if the workers’ environment makes it difficult or almost impossible to change their behaviour. This could also be the reason for the lower proportion of quitters among tobacco factory workers14.
In the present study, tobacco factory workers had a higher prevalence of periodontal pockets (47.5%) and loss of attachment (56.9%) compared to cotton ginning mill workers. The explanation for this difference could be the higher prevalence of smokeless tobacco use among tobacco factory workers, which is a potential risk factor for the development of periodontal pockets. Prevalence as high as 51% was reported for shallow pockets by Amjad et al.15 among tobacco chewers in Pakistan.
In the present study, tobacco-related oral mucosal lesions were seen only among tobacco factory workers. None of the cotton ginning mill workers exhibited tobaccorelated oral mucosal lesions. Among the oral mucosal lesions, the prevalence of tobacco pouch keratosis and leukoplakia were found to be 4.4% and 1.9%, respectively, for the tobacco factory workers. This could be due to the higher prevalence of tobacco use in chewing form (38.1%) than smoking form (25.6%) among the workers. Also, it could be that it takes prolonged exposure to develop leukoplakia while tobacco pouch keratosis develops earlier due to local irritation caused by the placement of quid16.
The mean overall OHIP-14 scores among tobacco factory workers and cotton ginning mill workers were 20.81±11.59 and 16.29±9.67, respectively. Similar findings were reported in a previous study conducted among the adult population in Chennai17. The explanation for the higher OHIP-14 score among tobacco factory workers could be attributed to their poor oral health status compared to cotton ginning mill workers.
A limitation of this study is that the socioeconomic status of the study subjects was not taken into account, as they were paid on a daily basis, which varied widely, making it difficult to calculate their monthly income.
CONCLUSIONS
The prevalence of periodontal diseases, oral mucosal lesions, use of tobacco and the OHIP-14 scores were all found to be significantly higher among tobacco factory workers compared to cotton ginning mill workers. OHIP-14 scores were significantly correlated with clinical oral health status indicators among subjects in both study groups. Hence, when planning treatment strategies, including tobacco cessation counselling for these workers, depending on the availability of resources and manpower, priority has to be given to the tobacco factory workers, as potentially malignant disorders and treatment needs are greater among this group compared to the cotton ginning mill workers. Therefore, an integrated curative and prevention based approach along with behaviour change programs, directed especially towards tobacco cessation, are warranted to achieve optimum level of oral health among these workers.