INTRODUCTION
The need to build resilient health systems has become increasingly evident in an era marked by unprecedented global challenges, such as the COVID-19 pandemic, natural disasters, and emerging infectious diseases. Health system resilience refers to the capacity of a healthcare system to withstand shocks, adapt to changing circumstances, and maintain essential functions during times of crisis. It encompasses the ability to respond effectively to emergencies, protect population health, and ensure continuity of care for all1-3.
Investing in health system resilience has become a priority for policymakers, healthcare leaders, and researchers worldwide, yet it remains a relatively new concept in the healthcare field4. While various definitions and theoretical frameworks are available, the practical application of this concept in health system research still needs to be improved5. The lessons learned from previous epidemics and pandemics highlight the substantial costs of inadequate preparedness, emphasizing the urgency to prioritize investments in prevention, health promotion, and coordinated global efforts1. More knowledge is needed regarding successful strategies to strengthen health system resilience in different contexts at local, national, and global levels, and this has been identified as a leading research priority.
Strengthening the underlying foundations of healthcare systems can enhance resilience, enabling better preparedness and response to natural disasters and disruptions. By addressing these challenges and investing in health system resilience, countries can strengthen their long-term sustainable socioeconomic growth, protect national security, and promote collective global health security. This scoping review aimed to provide a comprehensive overview and identify the key strategies for investing in health system resilience.
METHODS
Search strategy
This scoping review identified published literature and grey literature from PubMed and Google Scholar databases. A scoping review was chosen because of the heterogeneity of resilience strategies within the available research literature. A detailed search strategy is provided in Supplementary file Table A1. Briefly, the search was conducted between March 2020 and March 2023, covering topics related to health systems resilience. MeSH terms and free-text keywords were used to search for information on investment, financing, immunization/vaccination programs, resilience, and sustainability. Studies were identified if they were peer-reviewed and published in a scientific journal in English. In addition, the above systematic search was complimented by a grey literature search of relevant books, documents, government publications, and technical reports.
Study selection and data extraction
Inclusion and exclusion criteria are specified in Supplementary file Table A2. Studies were included if they were original research on the topics of health systems resilience and sustainability or if they were a review study of empirical research. Editorials, commentaries or opinion pieces or viewpoints, and articles not in English, were excluded.
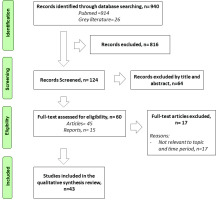
Publications from the PubMed database search were screened based on title and abstract. Two independent reviewers read selected articles in full and considered them for inclusion based on pre-established eligibility criteria. The screening and selection process is presented in Figure 1. Disagreements over including relevant publications were resolved through discussion with a third independent reviewer. Data were extracted on study characteristics, including study objectives, the primary topic the study focuses on, the summary of main findings, and the geographical focus categorized by WHO regions.
RESULTS
Completed in March 2023, the search yielded 940 relevant records. Of these, 60 full-text records were retrieved and reviewed. A total of 43 publications that met the inclusion criteria were included in the final sample (Figure 1). Of these studies, ten focused on the African Region6-15, seven on South-East Asian Region9,13,16-19, four on European Region2,19-21, six on Region of the Americas22-27, and nine studies did not have a specific geographical focus1,28-43. (Table 1)
Table 1
Detailed characteristics of studies included in this review (March 2020 - March 2023)
| Authors Year | Geographical focus | Primary topic | Study objective | Summary of main findings |
|---|---|---|---|---|
| Domapielle6 2021 | African Region (AFR) | Health financing models for universal health coverage in low- and middle-income countries | To determine the most suitable health financing model for achieving UHC in LMICs, this study aims to analyze empirical and theoretical discourses. It emphasizes the need for context-specific approaches, acknowledging the long-term policy engagement and adaptation to socio-cultural and political economy factors in implementing countries. | The analysis explores Ghana’s National Health Insurance Scheme implementation since 2003. Successful UHC relies on political support, economic stability, and a robust healthcare system. LMICs should learn from similar countries, develop tailored financing models, and build resilient health systems for UHC. It is an evolving process aligned with the WHO framework and SDG 3. |
| Mao et al.19 2020 | South-East Asian Region (SEAR) | Different pathways used to achieve UHC | To compare China and Vietnam’s approaches to achieving UHC through health insurance reform. | China focuses on expanding coverage through government subsidies, resulting in regional variations and limited-service coverage. In contrast, Vietnam aims for equitable UHC by providing a comprehensive service package for all enrollees. Both countries face challenges with income disparities and high catastrophic health expenditure rates. The study highlights the importance of political commitment, sustainable funding, and administrative capacity for successful UHC implementation. |
| Taylor et al.21 2022 | European Region (EUR) | Critical review of UK National Health Service data pertaining to doctors, nurses, midwives, and paramedics | This study examines challenges faced by the UK National Health Service healthcare workforce. | Demographic differences, service architecture issues, job stress, and high sickness absence rates are identified. Improving well-being requires considering sociocultural factors, service architecture, and developing inter-professional databases for long-term monitoring and multi-level strategies. |
| Myhre et al.20 2022 | European Region (EUR) | The role of national public health institutes | To explore how National Public Health Institutes bridge agendas by examining the strategies employed by these institutes. | Findings revealed five enabling factors critical to success: a strong legal foundation; scientific independence; public trust and legitimacy; networks and partnerships at global, national, and local levels; and stable funding. |
| Duff et al.24 2021 | Region of the Americas (AMR) | A global public health convention for the 21st century | To propose a new global public health security convention that enhances prevention, preparedness, and response to pandemic infectious diseases. | The study emphasizes the need for a new global public health security convention to enhance pandemic prevention and response. Ten recommendations are proposed, including empowering a global governing body, objective evaluation of national capacities, and stronger enforcement mechanisms. Overcoming barriers and fostering international collaboration are key for implementation. |
| Breneol et al.23 2022 | Region of the Americas (AMR) | Strategies to adapt and implement health system guidelines and recommendations | To map the evidence related to the adaptation and implementation of health system guidelines in low- and middle-income countries. | This review highlights the need for further research to enhance the implementation and adaptation of health system guidelines in low- and middle-income countries. The findings can guide future studies and emphasize the importance of collaboration across research, policy, and practice sectors to support local adaptation and implementation of guidelines in these settings. |
| Ifeagwu et al.7 2021 | African Region (AFR) | Health financing mechanisms in Sub-Saharan Africa | This systematic review aims to determine reported health financing mechanisms in SSA within the published literature and summarize potential learnings. | Collaborative efforts are required between local governments, donors, and private sectors to address the needs of vulnerable population groups. Adequate allocation of targeted resources and support from multiple stakeholders are essential to effectively meet the specific challenges faced by these populations. |
| Aslam et al.8 2022 | African Region (AFR) | Establishing a sustainable Healthcare environment in LMICs | This research aims to assess the effectiveness of initiatives aimed at enhancing training programs, living conditions, and financial security. The study seeks to explore the importance of implementing tailored financial models that consider the specific needs of each country. | Investing in the creation and retention of a local healthcare workforce is essential for improving healthcare systems. To achieve this, it is necessary to enhance training programs, living conditions, and financial security. It is important to recognize that a customized financial model is required for each country, as a uniform approach does not suit everyone’s specific needs. |
| Jakovljevic et al.17 2021 | South-East Asian Region (SEAR) | Political economy of health in financing and spending in the global south nations | To analyze the political economy of health spending in LMICs of the Global South, exploring historical trends, domestic manufacturing, and multinational pharmaceutical industries. Identify patterns, challenges, and driving forces. Assess the potential of cost-effectiveness-based decision-making and health technology assessment to address fiscal gaps and improve access to advanced medical technologies. | To strengthen medical technology manufacturing in LMICs, governments must invest in infrastructure, technology, and a skilled workforce. Evidence-based decision-making and health technology assessment play crucial roles in optimizing resource allocation and facilitating timely access to innovative treatments like monoclonal antibodies, biosimilars, and targeted oncology agents. |
| Siddiqi et al.9 2021 | South-East Asian Region (SEAR); African Region (AFR) | Global strategies and local implementation of health and health-related SDGs | This study highlights the early achievements, challenges, and opportunities for LMICs in implementing health and health-related sustainable development goals (HHSDGs). | Results indicate growing political commitment, strengthened monitoring systems, and engagement of development partners. However, limited involvement of civic society and academia, insufficient capacity development initiatives, and lack of a comprehensive communication strategy pose hurdles. Integration of non-health SDGs and multisectoral implementation strategies is crucial for accelerated HHSDG implementation. Further research and testing of interventions are recommended. |
| Saulnier et al.36 2021 | - | Health system resilience research agenda | To advance the understanding and application of health system resilience by addressing research gaps identified in existing frameworks. The study explores the measurement and management of dynamic performance, the interplay between societal and health system resilience, the influence of governance on resilience capacity, strategies for creating legitimacy, and the impact of the private sector on health system resilience. | This study emphasizes the importance of prioritizing research and development in the healthcare sector. By investing in research and development, governments can foster innovation, improve medical technologies, and drive economic growth. Collaboration with private and voluntary sectors is crucial for strengthening healthcare systems, leveraging expertise, and reaching vulnerable populations. Strong governance structures and policies are necessary to enhance resilience, streamline decision-making, and effectively respond to healthcare challenges. |
| Huffstetler et al.34 2022 | - | The impacts of donor transitions on health system in MICs | To examine and investigate the key factors necessary for a successful transition in healthcare programs. | Successful transition in healthcare programs requires strong leadership, comprehensive planning, and investments in financial, technical, and logistical capacity. Anticipating and addressing potential shortages and regularly monitoring the transition process are vital for mitigating challenges and ensuring program continuity, population health, and a seamless transition. |
| Forsgren et al.32 2022 | - | Health systems resilience in practice | To comprehensively examine the impact of donor transitions on health systems in MICs. The study aimed to identify the challenges, risks, and opportunities associated with donor exits. The study assessed the effects on different components of the health system, such as financial resources, medical products and supplies, service continuity, and human resources. | Successful transitions require strong leadership, comprehensive planning, and pre-transition investments in financial, technical, and logistical capacity. In the absence of such measures, shortages in resources, stock-outs, service disruptions, and workforce shortages negatively impact program continuity and population health. Understanding the interconnected ways in which donor transitions affect different components of the health system is crucial for effectively managing the risks and opportunities associated with donor exits in MICs. |
| Meyer et al.18 2020 | South-East Asian Region (SEAR) | A checklist to improve health system resilience | To create a checklist to measure the specific capacities, capabilities, and processes that health systems need in order to ensure resilience in the face of both infectious disease outbreaks and natural hazards. | Ten thematic categories play as crucial role in resilient health systems. These encompass core health system capabilities, infrastructure and transportation, financing, barriers to care, communication, collaboration, partnerships, leadership and command, surge capacity, risk communication, workforce, and infection control. These findings emphasize the importance of addressing these categories to establish and sustain resilient health systems capable of effectively responding to challenges and providing high-quality healthcare services. |
| Clarke et al.29 2022 | - | Costs of improving health emergency preparedness | To understand the cost associated with improving health emergency preparedness. The study aims to provide insights on the optimal level of investment and identify key areas of focus to enhance preparedness for health emergencies at the community and country levels. | To enhance global health emergency preparedness, substantial and sustained investments are necessary. Standardized methods for estimating investment sizes, along with transparent reporting of research methods, are crucial for interpreting and comparing studies. This will support estimating global resource needs and facilitate targeted investments to improve preparedness for future pandemics. |
| Taslakian et al.39 2022 | - | Diaspora involvement in health system strengthening | Examine the available literature to assess activities through which diasporas engage with the health system in their origin country and what barriers they face in their interventions. | Diaspora efforts addressed issues such as health workforce emigration, research and training capacity building, inadequate infrastructure, and finances. Activities included short-term missions, partnerships, return migration, research and training programs, and financial remittances. Barriers identified included financial needs, sustainability challenges, communication issues, lack of intention to return, infrastructure limitations, and political concerns. |
| Spicer et al.37 2020 | - | Why fragmentation persists in global health | To identify and describe the multiple causes of fragmentation in development assistance for health at the global level. The study aims to raise awareness and understanding of these causes and provide guidance for global health actors in addressing the problems of fragmentation and moving towards more synergistic approaches. The study is conducted as part of the Lancet Commission on Synergies between Universal Health Coverage, Health Security, and Health Promotion. | The study identifies five key factors that contribute to fragmentation in global health assistance: the proliferation of global health actors, challenges in global leadership, divergent interests, issues of accountability, and problems related to power relations. These factors hinder the harmonization of approaches and priorities among global health actors, prevent alignment with the needs of low- and middle-income countries, and perpetuate the use of funding instruments that further exacerbate fragmentation. |
| Debie et al.30 2022 | - | Successes and challenges of health systems | To synthesize the evidence and identify the successes and challenges of health systems governance in relation to achieving UHC and health security. The study aims to provide an understanding of the factors that contribute to the progress or hindrance in achieving UHC and health security through effective health systems governance. | Context-specific health policies, effective health financing, robust health intelligence, intersectoral collaboration, and accountability are key factors contributing to progress. Challenges include a one-size-fits-all approach, lack of funding, corruption, inadequate workforce, and weak regulatory policies. Decentralization, stakeholder support, resource distribution, independent accreditation, and integration of quality and equity indicators are recommended for advancing UHC and health security. |
| Jakab et al.35 2021 | Building the evidence base for global health policy: Strengthening institutional networks | To examine the role of national public health institutes and WHO collaborating centers in supporting public health system strengthening and generating evidence for health policy. The study aims to understand the global knowledge sources in public health and explore ways to invest in and utilize public health institutes and their capacities more effectively, particularly in light of the COVID-19 pandemic | Investing in public health and strengthening institutions can bring several benefits, including transparency, trust, socioeconomic dividends, collective health protection, and knowledge sharing. By prioritizing these areas and promoting collaboration, the study suggests actionable steps to develop and effectively utilize public health institutes and international networks. | |
| Hanney et al.33 2020 | Strengthening national health research systems | The main objective of the report is to emphasize the importance of high-quality research for improving population health and achieving the health-related Sustainable Development Goals. It aims to address the challenges faced in securing research funding, building research capacity, and utilizing resources effectively by advocating for a systems approach to strengthen national health research systems. | A report on health research systems strengthening highlights the importance of high-quality research for improving population health and achieving Sustainable Development Goals. Key findings include the need for a systems approach, involvement of health ministries, sustained political commitment, integration with the broader health system, contextual analysis, stakeholder engagement, monitoring and evaluation tools, and partnerships. | |
| Elnaiem et al.21 2023 | Global and regional governance of One Health and implications for global health security | To analyze the challenges and shortcomings in the global governance of One Health, particularly in relation to the COVID-19 pandemic. The study aims to identify and explore four key challenges: sectoral silos and tensions between human, animal, and environmental health; legal complexities and the impact of state sovereignty on governance; power dynamics and their influence on priority setting; and inadequate financing for epidemic prevention and preparedness. | To effectively address health emergencies and infectious diseases, efforts must target climate change, biodiversity loss, and land-use change, requiring legislation, investment, capacity building, and collaboration across sectors and professions. | |
| Tessema et al.10 2021 | African Region (AFR) | Preparedness, impact, and response on healthcare systems in Africa | To assess the existing evidence regarding the level of preparedness within the health systems, the impacts of COVID-19, and the responses to the pandemic in Africa. | The health systems in Africa were inadequately prepared for the pandemic. Interventions that will improve and strengthen health system resilience and financing through local, national, and global engagement should be prioritized. |
| Stubbs et al.38 2023 | The return of austerity imperils global health | To analyze the potential for increased national health budgets in low-income and middle-income countries to strengthen pandemic preparedness and response systems. By examining the new projections on public spending from the International Monetary Fund, this article assesses the feasibility of additional funding through domestic resource mobilization and the implications for global health security. | Domestic resource mobilization is now more important than ever to secure the necessary preparedness and resources. | |
| Tadesse et al.15 2021 | African Region (AFR) | Universal Health Coverage, health security and health promotion | To document and analyze the efforts made by Ethiopia to implement nationally synergistic approaches that unite the global health agendas of universal health coverage, health security, and health promotion. The study aimed to provide evidence of the successes achieved in the country’s health sector through the integration of these three key agendas. | Fragmentation of health system primarily manifested as inequities in access to health services, low health workforce and limited capacity to implementation guidelines. Donor driven vertical programs, multiple modalities of health financing, and inadequate multisectoral collaborations were also found to be key features of fragmentation. |
| Aftab et al.16 2020 | South-East Asian Region (SEAR) | Implementation of health and health-related sustainable development goals: progress | To examine the available evidence of implementation strategies being adopted by countries. | To expedite the implementation of health and health-related sustainable development goals (HHSDGs), crucial factors include enhancing the implementation of multisectoral efforts, building capacity, ensuring financial sustainability, and improving data availability. Strengthening these areas is essential to accelerate progress towards achieving the HHSDGs. |
| Evaborhene et al.14 2023 | African Region (AFR) | The Pandemic Treaty, the Pandemic Fund, and the Global Commons: our scepticism | To examine the implementation strategies adopted by countries to integrate and address the health-related goals within the broader framework of the Sustainable Development Goals (SDGs). By exploring the existing literature and available evidence, the study aims to fill the gap in understanding the practical approaches and strategies employed by countries to achieve the health-related targets of Agenda 2030. | Strengthening countries’ capacities requires increase in domestic investment. This article calls for wider structural reforms such as debt restructuring among other tools to strengthen countries’ capacities. |
| Balde et al.11 2022 | African Region (AFR) | Proposed framework for rethinking and rebuilding health systems | To evaluate the implementation and effectiveness of the transition framework proposed by the WHO Regional Office for Africa in building resilient health systems for future public health emergencies. The study aims to assess the extent to which the framework has been adopted by African countries and identify the challenges and successes encountered in its implementation. | The pandemic exposed healthcare inequalities and lack of preparedness in Africa. African countries have improved their response but need to strengthen health systems for future emergencies. The WHO Africa office proposes a framework that integrates science, data, technology, and research, prioritizes primary healthcare, and incorporates response into routine care. Equity, inclusiveness, and coherence are essential principles to ensure a resilient health system capable of addressing future crises while maintaining essential public health functions. |
| Kiendrébéogo et al.12 2021 | African Region (AFR) | Reinforcing locally led solutions for universal health coverage | Examines the effectiveness of new approaches in development assistance for health, focusing on low-income and middle-income countries transitioning to universal health coverage. It evaluates the African Collaborative for Health Financing Solutions (ACS) project’s impact, including five action steps, in Benin, Namibia, and Uganda, to inform future strategies. | The article presents new approaches for low-income and middle-income countries to gain control of their development assistance for health programs as they strive for universal health coverage (UHC). Based on the experience of the African Collaborative for Health Financing Solutions (ACS), the study suggests three paradigm shifts for development partners: emphasizing long-lasting processes, leveraging local expertise, and supporting practical resources. The study proposes five action steps to facilitate progress towards UHC, including aligning with country demand and strengthening accountability mechanisms. The ACS project has applied these steps in Benin, Namibia, and Uganda, showing promising preliminary achievements. |
| Paschoalotto et al.27 2023 | Region of the Americas (AMR) | Health system resilience | To examine the concept of resilience in the context of health systems by gathering insights from international experts. The study examined perspectives of international experts on various aspects of resilience, including concepts, stages, analytical frameworks, and implementation. | Existing studies on health system resilience have primarily examined high-income countries with robust systems or low-income countries with weak systems. However, it is crucial to broaden research to include middle-income countries with fragmented public and private sectors to enhance our understanding of health system resilience. |
| Alwan et al.13 2023 | South-East Asian Region (SEAR); African Region (AFR) | Successful design and transition to implementation of essential packages of health services | To examine the experiences of six low-income and lower middle-income countries in developing and implementing their own essential packages of health services (EPHS). | Four essential factors for effective Essential Public Health Services (EPHS): unwavering commitment, enduring funding, prepared health systems, and institutional integration. These prerequisites form the foundation for achieving successful EPHS implementation and ensuring public health initiatives are sustainable and impactful. |
| Zurynski et al.43 2022 | Western Pacific Region | How the health system cannot deliver sustainable performance | To develop an understanding of how the sustainable performance of healthcare systems (SPHS) has been conceptualized, defined, and measured. | Highlighted challenges in achieving SPHS due to complex patient populations, fragmented systems, and translational gaps. Strategies for improvement included fostering appropriate workplace cultures, involving communities and consumers, and adopting evidence-based practices and technologies. Long-term monitoring and evaluations were emphasized to adapt healthcare systems and anticipate future needs. |
| Braithwaite et al.28 2020 | Western Pacific Region | Transformational improvement in quality care and health systems | To analyze existing reports on quality gaps in health systems and move beyond mere conceptual diagnoses. The objective is to identify practical opportunities for transforming health systems by 2030. | Improving leadership and governance, utilizing proven information and communications technology effectively, providing more training and education for workforces, and implementing known strategies such as clinical practice guidelines and safe surgical checklists can enhance healthcare. The authors emphasize a patient-centered approach, implementing successful practices across different settings, and measuring progress over time. They stress the need for well-designed evaluations and a well-funded research program to support improvement efforts. |
| Preker et al.25 2021 | Multi-countries | Universal Health Coverage | Reviewed lessons learned about UHC in middle-income countries, with specific reference to achievements and challenges observed during recent years in four middle-income to upper middle-income countries. | Political sustainability, addressing the informal sector in UHC expansion, and supply-side challenges such as primary healthcare, provider pluralism, and the shortage of healthcare professionals. |
| Hamilton-West et al.51 2020 | European Region (EUR) | Supporting older people’s health: Social prescribing | To consider the potential role of social prescribing in supporting older people’s health and wellbeing. | Collaboration between researchers and planners to develop a stronger evidence base on the impacts of social prescribing. It calls for understanding variations in outcomes, implementing effective programs, and investing in allied initiatives to overcome barriers and support carers. The study concludes that social prescribing can benefit older adults’ health and wellbeing, but strategic alignment between research, implementation, policy, and investment is crucial for its success. |
| OECD (2023)2 | European Region (EUR) | Investing in health system resilience | To review the lessons learned from the COVID-19 pandemic and provide policy recommendations to enhance health system resilience in the face of future crises. | The report recommends policy changes in areas such as workforce, digitalization, continuity of care, mental health, long-term care, supply chains, and international cooperation to ensure global readiness for future crises. |
| Schneider et al.50 2021 | Multi-countries | Mirror, Mirror 2021: Reflecting on poor healthcare in the US compared to other high-income countries | To compare the performance of health care systems of 11 high-income countries. | The top-performing countries prioritize universal coverage, invest in primary care systems, reduce administrative burdens, and allocate resources to social services. |
| World Bank (2022)41 | Change cannot wait: Building resilient health systems in the shadow of COVID-19 | To develop a comprehensive framework for building resilient health systems in the face of increasing risks and future pandemics. By leveraging new research and incorporating the lessons learned from the COVID-19 pandemic, the study aims to provide practical guidance for countries and partners to enhance their health systems and improve health outcomes. | Invest in robust public health institutions, enhance early warning mechanisms, expand community health workforce, prioritize, and monitor investments, strengthen community engagement, and reshape health service delivery for better outcomes. | |
| WHO (2021)1 | Building health system resilience for UHC | WHO position paper on the extent to which the pandemic has disrupted health services, hindered progress towards Sustainable Development Goal 3 (SDG 3), and exacerbated existing inequalities. | Building a strong foundation in Primary Health Care is crucial, along with establishing institutionalized mechanisms for engaging the whole society. Additionally, creating an enabling environment for research innovation and learning is recommended. | |
| World Government Summit (2021)42 | Making healthcare systems resilient | To assess the weaknesses and vulnerabilities of current healthcare systems worldwide and propose strategies to enhance their resilience in the face of emerging health challenges. | Urgent measures are needed to enhance health system resilience and robustness in the healthcare sector, involving collaboration between governments, regulators, and healthcare providers. | |
| PAHO (2021)25 | Region of the Americas (AMR) | Strategy for building resilient health systems | To investigate and propose strategies for the transition from pandemic response to recovery in the Americas, with a focus on building sustainable and resilient health systems. | The critical path to recovery and progress toward the Sustainable Development Goals requires intensified actions to control the pandemic; adequate management of persons with COVID-19, including: the post COVID-19 condition experienced by some individuals; the rapid and equitable deployment of COVID-19 vaccines; and the mitigation of disruptions in the provision and availability of essential health services to protect health gains. |
| PAHO (2022)26 | Region of the Americas (AMR) | Building health system resilience for UHC: Americans | To assess the effectiveness of coordinated actions and systemic transformations in promoting universal access to health and universal health coverage, based on primary healthcare (PHC), in the Americas. | The need to transform health systems with a primary healthcare approach to facilitate pandemic recovery, sustain public health gains, and work towards universal health coverage. Key findings suggest strengthening leadership, governance, and stewardship, enhancing health service delivery networks, and increasing public financing for health and social protection, including addressing various determinants of health. |
| The Global Fund (2023)40 | Fighting pandemics and building a healthier and more equitable world | To investigate and propose strategies for fighting pandemics and build a healthier and more equitable world. | The key objectives to achieve success: 1) Enhancing health systems to address health threats effectively; 2) Maximizing the involvement of affected communities; 3) Promoting health equity, gender equality, and human rights; and 4) Mobilizing more resources to support the goals. | |
| Allin et al.22 2022 | Region of the Americas (AMR) | Sustainability and resilience in the Canadian health system | To provide evidence-based recommendations to inform decision-makers in the health sector in Canada. By identifying and addressing the critical issues faced by the Canadian health system, particularly those exacerbated by the COVID-19 pandemic, this study seeks to contribute towards improving the overall effectiveness, accessibility, and sustainability of healthcare services for all residents in Canada. | The report addresses and provide recommendation regarding governance, financing, workforce, technology, healthcare delivery, population health, and sustainability, emphasizing the need to strengthen collaborative actions, enhance transparency and role clarity across sectors, and increase investment in health innovation. |
Six main thematic areas were identified in the investment in building health system resilience (Figure 2). Of the six, the four thematic areas most frequently observed as strategies to invest in building a resilient health system were: 1) Multisectoral coalition and collaboration, 2) Prioritization of future research, 3) Creating a sustainable healthcare workforce, and 4) Governance and leadership. The other two were: 5) Investing in preventive care, and 6) Domestic resource mobilization. Table 2 outlines in detail the six thematic areas for investing in health system resilience, and gives examples from the literature.
Table 2
Summary findings and description of main themes identified for sustainable and resilient health system, including examples from the literature
| Themes identified | Description | Examples from literature |
|---|---|---|
| Investing in preventive care (n=13) | The development of primary healthcare structures, service delivery and comprehensive and accessible services to individuals and communities | Investing in primary healthcare structure Aslam et al. 20228, Meyer et al. 202018, Preker et al. 202125, OECD 20232, Schneider et al. 202150, World Bank 202241, WHO 20211, PAHO 202125, PAHO 202226, The Global Fund 202340 Investing in disease prevention Aslam et al. 20228, Hamilton-West et al. 202051, PAHO 202125, PAHO 202226 |
| Governance and leadership (n= 18) | Political commitment, policies, government subsidies, empowering global government bodies and foster innovation and power dynamics | Political commitment/government/leadership/judicial decision-making Domapielle 20216, Mao et al. 202019, Siddiqi et al. 20219, Saulnier et al. 202136, Huffstetler et al. 202234, Forsgren et al. 202232, Meyer et al. 202018, Debie et al. 202230, Alwan et al. 202313, Braithwaite et al. 202028, Preker et al. 202125, OECD 20232 WHO 20211, World Government Summit 202142, PAHO 202125, PAHO 202226, The Global Fund 202340, Allin et al. 202222 |
| Domestic resource mobilization (n=9) | Strengthen domestic manufacturing capacity of medical technologies, pharmaceuticals, infrastructure, transportation, technology and information and addressing income levels, a robust economy, a broader tax base | Strong capacity to mobilize taxes, domestic resource mobilization Domapielle 20216, Stubbs et al. 202338, Mao et al. 202019 Strengthen domestic manufacturing capacity of medical technologies/devices and pharmaceuticals/technical and logistical capacity Jakovljevic et al. 202117, Huffstetler et al. 202234, Jakab et al. 202135 and Infrastructure/Transportation, technology, and information Meyer et al. 202018, Paschoalotto et al. 202327, Braithwaite et al. 202028 |
| Multisectoral coalition and collaboration (n=24) | Establishing coalition, networks, and partnerships at global, national, and local levels. Pooling of resources, sharing of expertise. Exchange of valuable insights, alignment of priorities, and coordinating interventions by enhancing communication channels and implementing collaborative decision-making processes. Investing in comprehensive communication strategies and prevention of fragmentation | Establishing coalition, networks and partnerships at global, national and local levels/multisectoral collaboration/communications, prevention of fragmentation Mao et al. 202019, Breneol et al. 202223, Myhre et al. 202220, Ifeagwu et al. 20217, Siddiqi et al. 20219, Saulnier et al. 202136, Meyer et al. 202018, Spicer et al. 202037, Debie et al. 202230, Jakab et al. 202136, Elnaiem et al. 202321, Tadesse et al. 202115, Evaborhene et al. 202314, Balde et al. 202211, Kiendrébéogo et al. 202112, Paschoalotto et al. 202327, Alwan et al. 202313, Zurynski et al. 202243, Braithwaite et al. 202028, OECD 20232, WHO 20211, PAHO 202226, The Global Fund 202340, Allin et al. 202222 |
| Prioritization of future research (n=23) | Investing in monitoring and evaluation, enhancement in data visibility, data technology, availability, and the translational gap in evidence to practice. Investment in research and training programs | Prioritization of future research/monitoring and evaluation/investing in data visibility/availability/translational gap in evidence to practice Breneol et al. 202223, Ifeagwu et al. 20217, Aslam et al. 20228, Jakovljevic et al. 202117, Siddiqi et al. 20219, Saulnier et al. 202136, Huffstetler et al. 202234, Forsgren et al. 202232, Clarke et al. 202229, Taslakian et al. 202239, Debie et al. 202230, Jakab et al. 202135, Hanney et al. 202033, Tessema et al. 202110, Aftab et al. 202016, Kiendrébéogo et al. 202112, Zurynski et al. 202243, Braithwaite et al. 202028, OECD 20232, WHO 20211, World Government Summit 202142, PAHO 202226, The Global Fund 202340 |
| Creating a Sustainable Healthcare workforce (n=19) | Investing in strategies that improve well-being and Workforce Management/supporting capacity building and the development of inter-professional national databases | Creating a Sustainable Healthcare workforce through strategies that improve well-being and Workforce Management/supporting capacity building Domapielle 20216, Myhre et al. 202220, Taylor et al. 202221, Breneol et al. 202223, Aslam et al. 20228, Siddiqi et al. 202119, Huffstetler et al. 202234, Forsgren et al. 202232, Tessema et al. 202110, Tadesse et al. 202115, Aftab et al. 202016, Zurynski et al. 202243, Braithwaite et al. 202029, OECD 20232, World Government Summit 202142, PAHO 202125, PAHO 202226 Development of inter-professional national databases Breneol et al. 202223, Duff, Liu et al. 202124, Allin et al. 202222 |
Investing in preventive care
The development of primary healthcare structures is essential for building resilient health systems, as outlined in the World Health Organization’s Framework on Integrated People-Centered Health Services45. A well-functioning primary healthcare system is pivotal in improving health system resilience during emergencies and disease outbreaks. The primary healthcare system is a foundation for a robust and adaptable health system that can effectively respond to various challenges and ensure the well-being of individuals and communities1,2,8,21,26,41,42,46. Authors suggested that investing in preventive measures, such as early detection, disease prevention, and health promotion, can significantly reduce the burden on healthcare systems. By investing in primary healthcare structures and disease prevention initiatives, health systems can identify health issues early, minimize the prevalence and impact of diseases, and enhance their overall resilience8,19,25,26. These studies highlight why building a solid foundation of primary health care and establishing an institutionalized mechanism for engaging the whole society is crucial to improve population health outcomes. This enables early identification of health risks, prompt interventions, and the management of chronic conditions, leading to better health outcomes and reduced healthcare costs in the long-term.
Governance and leadership
Effective governance and leadership were recurring themes in the literature. Political commitment, government, and leadership in healthcare governance are critical in building a resilient health system that can achieve universal health coverage (UHC), attaining Sustainable Development Goal 3, and ensuring successful transitions in healthcare programs and donor exists. The analysis of Domapielle6 of Ghana’s National Health Insurance Scheme (NHIS) implementation, emphasized the need for political support, economic stability, and a robust healthcare system for UHC. Similarly, Mao et al.19 underscored the significance of political commitment, sustainable funding, and administrative capacity in achieving equitable UHC, drawing lessons from China and Vietnam. Siddiqi et al.9 emphasized the need for political commitment, capacity development, and multisectoral strategies to accelerate the implementation of health-related Sustainable Development Goals (HHSDGs) in low middle-income countries (LMICs). Huffsteler et al.34 highlighted that ineffective leadership during donor transitions in middle-income countries (MICs) has significant consequences, often leading to disruptions and premature termination of health programs. They argued that a successful transition of healthcare programs, particularly in areas such as HIV/AIDS, immunization programs such as the Global Fund to Fight AIDS, Tuberculosis and Malaria, Gavi, and the Vaccine Alliance, requires strong leadership and comprehensive planning. Numerous studies and reports have emphasized the importance of strong political commitment and effective governance in healthcare systems1,2,6,9,13,18,19,22,25,26,28,30,32,34,36,40,42,45. They argued that judicial decision-making, government support, and leadership are essential for establishing and sustaining effective healthcare policies and initiatives. Likewise, successful healthcare transitions, managing risks associated with donor exits, and establishing resilient health systems require comprehensive planning, infrastructure, financing, communication, and leadership.
Domestic resource mobilization
Strengthening the domestic manufacturing capacity of medical technologies, devices, and pharmaceuticals and improving technical and logistical capacity were highlighted as essential in building a health system’s resilience6,17-19,27,28,34,35,38. The need for broader structural reform, including debt restructuring17, the role of evidence-based decision-making and health technology (HTA) in optimizing resource allocation could ensure timely access to innovative treatments contributing to the overall health system. Jakovljevic et al.17 argued that governments must invest in infrastructure and technology to strengthen medical technology manufacturing in low- and middle-income countries. Likewise, Huffstetler et al.34 and Paschoalotto et al.27 emphasized the need to enhance domestic manufacturing capabilities to reduce import dependence and ensure a stable supply of essential healthcare resources17,27,34. Additionally, investment in infrastructure, transportation, technology, and information, as advocated by Meyer et al.18 and Braithwaite et al.28 are crucial to improve health system resilience to infectious disease outbreaks and transform the quality of care through the delivery of efficient healthcare services. Stubbs et al.38 similarly argued that with significant increases in national health budgets through domestic resource mobilizations, low-income and middle-income countries can avoid deteriorating population health and weakened public health services due to austerity measures driven by rising debt repayments and economic hardships.
Improved multisectoral communication, partnerships, and collaboration
Establishing global, national, and local coalitions, networks, and partnerships is crucial for promoting coordinated efforts and information sharing. Multisectoral communication, partnerships, and collaboration are essential in preventing fragmentation and building a resilient health system, ensuring a holistic approach to healthcare, and attaining a sustainable performance of healthcare systems (SPHS)1,2,7,9,11-15,18,29,20,22,23,26-28,30,31,35-37,40,43. Fragmentation can hinder effective responses and undermine the overall capacity of the health system. According to the findings of Spicer et al.37, fragmentation poses a significant challenge in LMICS nations, compounded by many global health actors with divergent interests and inadequate accountability and leadership. They advocated for strategic communication and collaboration as crucial measures to enhance existing programs instead of initiating new ones. Furthermore, they suggest that high-income countries should allocate funds towards multilateral initiatives to mitigate the parallel bilateral programs they support38. Debie et al.30, Kiendrebeogo et al.12, and Allin et al.22 highlighted that by enhancing communication channels, stakeholders could exchange valuable insights, align priorities, and coordinate interventions, ensuring efficient resource allocation and comprehensive response to health emergencies, subsequently strengthening the resilience of the health system.
Prioritization of future research and data visibility
Investing in research and data visibility is crucial for improving the resilience of health systems. By prioritizing these areas, health systems can proactively identify and address knowledge gaps, make evidence-based decisions, and continuously learn and improve.
The reviewed literature emphasizes the need to prioritize future research, monitoring, and evaluation in healthcare systems. Research investment generates new insights, expands scientific knowledge, and identifies innovative approaches to healthcare delivery. This facilitates evidence-based decision-making and informs policy development, ensuring health systems have up-to-date information and practical strategies to respond to evolving health challenges1,40-43. Additionally, prioritizing research on building health system resilience allows identifying best practices, effective interventions, and strategies for building adaptive and robust health systems.
Improving data visibility is equally vital in building health system resilience, as reported by Breneol et al.23, Ifeagwu et al.7, and Aslam et al.8. Accessible and high-quality data are necessary for monitoring health trends, identifying service delivery gaps, and evaluating the impact of interventions. Investing in data collection, management, and analysis enables health systems to generate timely and accurate information to inform decision-making processes. Data visibility also promotes cross-sectoral collaboration and knowledge sharing, enabling stakeholders to collaborate based on a shared understanding of health system challenges and priorities7,8,15,23. The studies by Hanney et al.33 and OECD (2023)2 similarly called for comprehensive research prioritization frameworks to guide the allocation of resources and efforts in healthcare research.
To effectively address the evolving health needs of populations, governments and policymakers must prioritize research investment and data infrastructure. Focusing on these areas will equip health systems with the knowledge and information necessary to build resilience, respond to emerging health challenges, make evidence-based decisions, and foster continuous learning and improvement1,2,25,26,41.
Creating a sustainable healthcare workforce
Creating a sustainable healthcare workforce was identified as a key investment for building health system resilience that ensures high-quality care delivery2,6,8,9,15,16,20-26,28,32,34,42,43. Taylor et al.21 highlighted that improving well-being requires considering sociocultural factors, service architecture, and developing inter-professional databases for long-term monitoring. Domapielle et al.6 and Myhre et al.20 emphasized supporting healthcare professionals’ well-being and providing adequate resources for workforce leadership and management practices. Developing inter-professional national databases, as advocated by Breneol et al.23 and Duff et al.24, can enhance collaboration and coordination among different healthcare professionals. Expanding the community health workforce while investing in training and education, and improving healthcare worker’s well-being, will improve the healthcare system2,25,26,27.
DISCUSSION
This review aimed to provide a comprehensive overview of the key factors contributing to the investment in building health system resilience. As noted above, we observed several emerging themes, including investing in preventive care, prioritizing future research, creating a sustainable healthcare workforce, promoting multisectoral coalition and collaboration, strengthening governance and leadership, and mobilizing domestic resources. Investing in these factors collectively could strengthen health systems, enabling them to withstand and respond to natural hazards, disruptions, and high demands.
Investing in preventive care emerges as a crucial strategy to reduce the burden on healthcare systems and enhance overall resilience. Despite mounting evidence demonstrating the efficacy of cost-effective health promotion and disease prevention measures in enhancing health outcomes, a small portion of total health expenditure is currently directed towards such preventive activities46. By focusing on protection, prevention and health promotion as established in the World Federation of Public Health Associations (WFPHA) Global Charter47, we can strive for a healthcare system that emphasizes control of communicable diseases, emergency preparedness, occupational and environmental health sustainability, vaccination, screening, and effective disease management interventions. Furthermore, we can create a health system that promotes behavior change, enhance health literacy, and addresses social and environmental determinants of health. Through early detection, disease prevention, and health promotion, health systems can identify health issues at an early stage, minimize disease prevalence and impact, and improve their capacity to respond to crises2,25,26. This finding underscores the importance of primary healthcare structures and disease prevention initiatives as essential components of a resilient health system. The role of effective governance and leadership in building health system resilience is emphasized in this review. The findings highlight the need for political commitment, sustainable funding, administrative capacity, and comprehensive planning to establish and sustain effective healthcare policies and initiatives. This implies that resilient health systems are not solely dependent on the availability of resources but also require strong leadership and governance structures to guide and implement policies effectively1,40,41,48. Another significant investment strategy identified in this review is the importance of domestic resource mobilization. Health systems can establish a stable and reliable funding base for healthcare services by strengthening the capacity to generate and mobilize taxes and domestic resources. This reduces dependence on imports and enhances the availability of essential healthcare resources, ensuring a consistent supply even during disruptions17,34,35. Additionally, investing in infrastructure, transportation, technology, and information systems plays a crucial role in enabling efficient healthcare delivery and contributes to the overall resilience of the health system.
Multisectoral collaboration and partnerships are important strategies for building resilient health systems, particularly in low- and middle-income countries (LMICs). The policy and planning meeting for the WHO’s Africa region in 2020 similarly emphasized the importance of this approach in improving health system resilience49. Preventing fragmentation enhances the efficiency and effectiveness of interventions, promoting a cohesive and streamlined approach to health system strengthening1,44. This integrated approach fosters seamless transitions between different levels of care, improving the overall patient experience and health outcomes. Health systems can enhance their preparedness and response capacity by fostering collaboration and communication at global, national, and local levels, preventing the duplication of health programs, and leading to more efficient use of resources. Multisectoral collaboration promotes a holistic approach to healthcare, facilitating effective interventions and improving overall health system performance4,48. Another strategy is investing in future research and data infrastructure, which is a proactive approach to addressing knowledge gaps, making evidence-based decisions, and continuously improving health system resilience. By prioritizing research and improving data visibility and availability, health systems can improve containment and mitigation efforts, including early warning systems, and ensure patients receive the proper care for their needs2. Health systems can stay updated on emerging health challenges, identify best practices, and adapt their strategies accordingly. This underscores the importance of a learning and adaptive approach to building resilient health systems.
Limitations
There are limitations to consider when interpreting the findings from this study. While some strategies may fit into multiple themes, the review only presents each strategy once in the most relevant thematic area, potentially oversimplifying their complexity and interconnectedness across different themes. This approach could result in a limited understanding of their variations and potential overlap, missing out on nuances and interactions. Additionally, the study’s use of descriptive analysis to examine strategies may not provide a complete understanding of their impact. The review utilized PubMed and Google Scholar as primary databases for data retrieval. However, it is acknowledged that including other supplementary databases, could have augmented the breadth of literature coverage. Furthermore, due to inherent heterogeneity observed across the studies included in our analysis, conducting a quality appraisal proved challenging and thus emerged as a limitation within our study. Finally, by focusing exclusively on articles published from March 2020 onwards, the study may have overlooked relevant studies published before this period, limiting the historical context and the understanding of the identified strategies.
CONCLUSIONS
A comprehensive approach that covers various strategies is necessary to achieve a resilient health system. This involves investing in preventive care, strengthening governance and leadership, mobilizing domestic resources, promoting multisectoral collaboration, prioritizing future research, and creating a sustainable healthcare workforce. By implementing these strategies, policymakers, healthcare leaders, and researchers can bolster the nation’s ability to endure shocks, adapt to evolving circumstances, sustain essential functions during times of crisis and safeguard public health and contribute to sustainable socioeconomic development and global health security.