Home
Issues
Aim and Scope
Open Access
Editorial Board
Indexing
Why publish with us
Contact Us
Instructions to Authors (PDF)
Manuscript Types
Manuscript Formatting
How to submit
Preprints
Special publications & Reprints
Authorship & COI
Principles of Transparency Checklist
Data Policies
Publication Ethics and Publication Malpractice Statement
RESEARCH PAPER
Burden of tobacco, kola nut and alcohol consumption
and its association with periodontal disease, potentially
malignant lesions and quality of life among bus drivers,
Lagos State, Nigeria
1
Lagos State University College of Medicine, Ikeja, Nigeria
2
Department of Paediatrics, Amuwo Odofin Maternal and Child Centre,
Festac, Nigeria
3
Department of Oral Pathology and Oral Medicine, Lagos State University
Teaching Hospital, Ikeja, Nigeria
Submission date: 2020-01-10
Final revision date: 2020-02-03
Acceptance date: 2020-03-03
Publication date: 2020-03-23
Corresponding author
Afolabi Oyapero
Lagos State University College of Medicine, 1-5 Oba Akinjobi Way, Ikeja, Lagos, Nigeria
Lagos State University College of Medicine, 1-5 Oba Akinjobi Way, Ikeja, Lagos, Nigeria
Popul. Med. 2020;2(March):5
KEYWORDS
TOPICS
ABSTRACT
Introduction:
To improve their performance and alertness, bus drivers are known to abuse alcohol, cigarette, kola nut and other substances that have substantial independent and combined deleterious effects on oral tissues. The study aimed to characterize risk associations between aggregates of alcohol/tobacco use and oral-health outcomes among a group of road transport workers in the Ojota and Berger bus terminals in Lagos State.
Methods:
Data were obtained from a probability sample of 150 commercial drivers from two bus terminals (Ojota and Berger) in Lagos State via face-to-face interviews and oral examination using a validated structured questionnaire. Multistage cluster sampling was conducted through the selection of two clusters from the major registered motor parks at the first stage by simple random sampling; while the selection of drivers was done by simple random sampling (balloting), using the list of registered drivers in the two garages as the sampling frame. Past and present tobacco and alcohol use were self-reported by respondents. Multivariable regression analysis measured the relationship between the outcomes [potentially malignant lesions (Leukoplakia, Erythroplakia, Smokers palate, Lichen planus), periodontal disease (CPITN Scores 3,4) and oral-health-related quality of life, OHRQoL (OHIP-14)] and exposures, controlling for the covariates age, marital status, education status, income level, oral hygiene, dental caries, functional tooth units, and previous treatment.
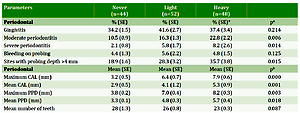
Results:
All the respondents were male. The prevalence of alcohol ever use was 82%, and 35% were moderate or heavy drinkers (2–4 drinks). Prevalence of tobacco ever use was 71%; while 32% were heavy smokers (>11 cigarettes/ day), 64% had a history of kola nut chewing habit, and 53% ate at least 2 kola nuts daily. Heavy smokers had more potentially malignant lesions (OR=1.89, 95% CI: 1.33–3.27); significantly worse periodontal destruction (OR=3.12, 95% CI: 2.28–5.17); and significantly worse OHRQoL (OR=2.35, 95% CI: 1.42–4.54). For individual OHRQoL domains, Pain 3.03 ( 95% CI: 1.77–4.21], Discomfort 2.89 [ 95% CI: 2.32– 4.17], Speech 3.02 ( 95% CI: 2.32–4.13), Diet 2.77 (95% CI: 1.87–4.28), Embarrassment 1.97 (95% CI: 1.65–3.14) and Self-consciousness 2.34 (95% CI: 1.93–3.48), were significantly associated with heavy smoking, after controlling for covariates.
Conclusions:
This study highlights the role of tobacco and alcohol as modifiable risk factors for periodontal disease and potentially malignant lesions that can impact negatively on OHRQoL. Bus drivers, in Lagos State, Nigeria, are an important target group in controlling tobacco and alcohol use in Nigeria and should receive adequate attention for oral health promotion and other preventive initiatives.
To improve their performance and alertness, bus drivers are known to abuse alcohol, cigarette, kola nut and other substances that have substantial independent and combined deleterious effects on oral tissues. The study aimed to characterize risk associations between aggregates of alcohol/tobacco use and oral-health outcomes among a group of road transport workers in the Ojota and Berger bus terminals in Lagos State.
Methods:
Data were obtained from a probability sample of 150 commercial drivers from two bus terminals (Ojota and Berger) in Lagos State via face-to-face interviews and oral examination using a validated structured questionnaire. Multistage cluster sampling was conducted through the selection of two clusters from the major registered motor parks at the first stage by simple random sampling; while the selection of drivers was done by simple random sampling (balloting), using the list of registered drivers in the two garages as the sampling frame. Past and present tobacco and alcohol use were self-reported by respondents. Multivariable regression analysis measured the relationship between the outcomes [potentially malignant lesions (Leukoplakia, Erythroplakia, Smokers palate, Lichen planus), periodontal disease (CPITN Scores 3,4) and oral-health-related quality of life, OHRQoL (OHIP-14)] and exposures, controlling for the covariates age, marital status, education status, income level, oral hygiene, dental caries, functional tooth units, and previous treatment.
Results:
All the respondents were male. The prevalence of alcohol ever use was 82%, and 35% were moderate or heavy drinkers (2–4 drinks). Prevalence of tobacco ever use was 71%; while 32% were heavy smokers (>11 cigarettes/ day), 64% had a history of kola nut chewing habit, and 53% ate at least 2 kola nuts daily. Heavy smokers had more potentially malignant lesions (OR=1.89, 95% CI: 1.33–3.27); significantly worse periodontal destruction (OR=3.12, 95% CI: 2.28–5.17); and significantly worse OHRQoL (OR=2.35, 95% CI: 1.42–4.54). For individual OHRQoL domains, Pain 3.03 ( 95% CI: 1.77–4.21], Discomfort 2.89 [ 95% CI: 2.32– 4.17], Speech 3.02 ( 95% CI: 2.32–4.13), Diet 2.77 (95% CI: 1.87–4.28), Embarrassment 1.97 (95% CI: 1.65–3.14) and Self-consciousness 2.34 (95% CI: 1.93–3.48), were significantly associated with heavy smoking, after controlling for covariates.
Conclusions:
This study highlights the role of tobacco and alcohol as modifiable risk factors for periodontal disease and potentially malignant lesions that can impact negatively on OHRQoL. Bus drivers, in Lagos State, Nigeria, are an important target group in controlling tobacco and alcohol use in Nigeria and should receive adequate attention for oral health promotion and other preventive initiatives.
REFERENCES (39)
1.
Landsbergis PA, Grzywacz JG, LaMontagne AD. Work organization, job insecurity, and occupational health disparities. Am J Ind Med. 2014;57(5):495-515. doi:10.1002/ajim.22126
2.
Gay Anderson D, Riley P. Determining standards of care for substance abuse and alcohol use in long-haul truck drivers. Nurs Clin North Am. 2008;43(3):357-365. doi:10.1016/j.cnur.2008.04.003
3.
Zhang X, Chow EP, Wilson DP, Sun X, Zhao R, Zhang J, Jing J, Zhang L. Prevalence of HIV and syphilis infections among long-distance truck drivers in China: A data synthesis and meta-analysis. Int J Infect Dis. 2013;17(1):e2–e7. doi:10.1016/j.ijid.2012.07.018
4.
Singh RK, Joshi HS. Sexual behavior among truck drivers. Indian J Public Health. 2012;56(1):53-56. doi:10.4103/0019-557x.96976
5.
Nascimento EC, Nascimento E, Silva Jde P. Alcohol and amphetamines use among long-distance truck drivers. Rev Saude Publica. 2007;41(2):290-293. doi:10.1590/S0034-89102007000200017
6.
Labat L, Fontaine B, Delzenne C, et al. Prevalence of psychoactive substances in truck drivers in the Nord-Pas-de-Calais region (France). Forensic Sci Int. 2008;174(2-3):90-94. doi:10.1016/j.forsciint.2007.03.004
7.
Ebrahimi MH, Delvarianzadeh M, Saadat S. Prevalence of metabolic syndrome among Iranian occupational drivers. Diabetes Metab Syndr. 2016;10(1):S46-S51. doi:10.1016/j.dsx.2015.09.011
8.
Saini GK, Gupta ND, Prabhat KC. Drug addiction and periodontal diseases. J Indian Soc Periodontol. 2013;17(5):587–591. doi:10.4103/0972-124x.119277
9.
Yanagisawa T, Ueno M, Shinada K, Ohara S, Wright FA, Kawaguchi Y. Relationship of smoking and smoking cessation with oral health status in Japanese men. J Periodontal Res. 2019;45(2):277–283. doi:10.1111/j.1600-0765.2009.01233.x
10.
Leung WK Ng DK, Jin L, Corbet EF. Tooth loss in treated periodontitis patients responsible for their supportive care arrangements. J Clin Periodontol. 2006;33(4):265–575. doi:10.1308/135576106778529044
11.
da Silva ACF, Luiz RR, Leão AT. The relationship between alcohol dependence and periodontal disease. J Periodontol. 2008;79(6):993–998. doi:10.1902/jop.2008.070525
12.
Marr JJ, Spilberg I. A mechanism for decreased resistance to infection by gram-negative organisms during acute alcoholic intoxication. J Lab Clin Med. 1975;86(2):253–258. PMID:807663.
13.
Khocht A, Janal M, Schleifer S, Keller S. The influence of gingival margin recession on loss of clinical attachment in alcohol-dependent patients without medical disorders. J Periodontol. 2003;74(4):485–493. doi:10.1902/jop.2003.74.4.485
14.
Neville BW, Day TA. Oral cancer and pre-cancerous lesions. CA Cancer J Clin 2002;52(4):195-215. doi:10.3322/canjclin.52.4.195
15.
Mello FW, Melo G, Pasetto JJ, Silva CAB, Warnakulasuriya S, Rivero ERC. The synergistic effect of tobacco and alcohol consumption on oral squamous cell carcinoma: a systematic review and meta-analysis. Clin Oral Investig. 2019;23(7):2849-2859. doi:10.1007/s00784-019-02958-1
16.
Melrose RJ. Premalignant oral mucosal diseases. J Calif Dent Assoc. 2001;29:593–600. PMID:11577670.
17.
Hashibe M, Sankaranarayanan R, Thomas G, et al. Body mass index, tobacco chewing, alcohol drinking and the risk of oral submucous fibrosis in Kerala, India. Cancer Causes Control. 2002;13(1):55-64. doi:10.1023/a:1013991025848
18.
Hashibe M, Mathew B, Kuruvilla B, et al. Chewing tobacco, alcohol, and the risk of erythroplakia. Cancer Epidemiol Biomarkers Prev. 2000;9(7):639–645. PMID:10919731.
19.
Benedetti G, Campus G, Strohmenger L, Lingström P. Tobacco and dental caries: a systematic review. Acta Odontol Scand. 2013;71(3–4):363–371. doi:10.3109/00016357.2012.734409
20.
Millar W J, Locker D. Smoking and oral health status. J Can Dent Assoc. 2007;73(2):155. PMID:17355806.
21.
Maida C A, Marcus M, Spolsky V W, Wang Y, Liu H. Sociobehavioral predictors of self-reported oral health-related quality of life. Qual Life Res. 2013;22(3):559–566. doi:10.1007/s11136-012-0173-z
22.
Åstrøm AN, Ekback G, Ordell S, Unell L. Social inequality in oral health-related quality of life, OHRQoL, at early older age: evidence from a prospective cohort study. Acta Odontol Scand. 2011;69(6):334–342. doi:10.3109/00016357.2011.568965
23.
Lagos State Ministry of Science and Technology, Lagos State Government. About Lagos. 2018. https://lagosstate.gov.ng/abou.... Accessed October 8, 2019.
24.
Sreedevi M, Ramesh A, Dwarakanath C. Periodontal status in smokers and nonsmokers: a clinical, microbiological, and histopathological study. Int J Dent. 2012;2012:1-10. doi:10.1155/2012/571590
25.
Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25(4):284-290. doi:10.1111/j.1600-0528.1997.tb00941.x
26.
Kramer IR, Pindborg JJ, Bezroukov V, Infirri JS. Guide to epidemiology and diagnosis of oral mucosal diseases and conditions. World Health Organization. Community Dent Oral Epidemiol. 1980;8(1):1–26. doi:10.1111/j.1600-0528.1980.tb01249.x
27.
Tse JLM, Flin R, Mearns K. Bus driver well-being review: 50 years of research. Transportation Research Part F: Traffic Psychology and Behaviour. 2006;9(2):89–114. doi:10.1016/j.trf.2005.10.002
28.
Benavides FG, Benach J, Mira M, Sáez M, Barceló A. Occupational categories and sickness absence certified as attributable to common diseases. Eur J Public Health. 2003;13(1):51-55. doi:10.1093/eurpub/13.1.51
29.
Jornet PL, Garcia FJ, Berdugo ML, Perez FP, Lopez AP. Mouth self-examination in a population at risk of oral cancer. Aust Dent J. 2015;60(1):59-64. doi:10.1111/adj.12274
30.
Aniebue PN, Okonkwo KOB. Prevalence of psychoactive drug use by taxi drivers in Nigeria. J College Med. 2008;13(3):48-52. doi:10.3126/jcmsn.v13i3.18403
31.
Lasebikan VO, Gureje O. Lifetime and 7-day alcohol consumption in the elderly, prevalence and correlates: Reports from the Ibadan Study of Aging. Afr J Med Med Sci. 2015;44(1):33-41. PMID:26548114.
32.
Young LA, Young LG, Klein MM, Klein DM, Beyer D. Recreational drugs. New York, NY: Macmillan Pub Co; 1985.
33.
Galanter M. Innovations: alcohol & drug abuse: spirituality in Alcoholics Anonymous: a valuable adjunct to psychiatric services. Psychiatr Serv. 2006;57(3):307-309. doi:10.1176/appi.ps.57.3.307
34.
Choi B, Schnall P, Dobson M, Yang H, Baker D, Seo Y. A socioecological framework for research on work and obesity in diverse urban transit operators based on gender, race, and ethnicity. Annals of Occupational and Environmental Medicine. 2017;29(1):15. doi:10.1186/s40557-017-0171-2
35.
Dietrich T, Bernimoulin J-P, Glynn R. The effect of cigarette smoking on gingival bleeding. J Periodontol. 2004;75(1):16–22. doi:10.1902/jop.2004.75.1.16
36.
Grossi SG, Genco RJ, Machtei EE, et al. Assessment of risk for periodontal disease: II: Risk indicators for alveolar bone loss. J Periodontol. 1995;66(1):23–29. doi:10.1902/jop.1995.66.1.23
37.
Benowitz NL. Pharmacology of nicotine – addiction and therapeutics. Annu Rev Pharmacol Toxicol. 1996;36(1):597–613. doi:10.1146/annurev.pa.36.040196.003121
38.
Warnakulasuriya S, Ariyawardana A. Malignant transformation of oral leukoplakia: a systematic review of observational studies. J Oral Pathol Med. 2016;45(3):155-166. doi:10.1111/jop.12339
39.
Hämäläinen J, Kaprio J, Isometsä E, Heikkinen M, Poikolainen K, Lindeman S, Aro S. Cigarette smoking, alcohol intoxication and major depressive episode in a representative population sample. J Epidemiol Community Health. 2001;55(8):573–576. doi:10.1136/jech.55.8.573
CITATIONS (6):
1.
Are Nigerian oral health workers overlooking opportunities to promote interventions for tobacco smoking cessation?
Afolabi Oyapero, Olubukola Olatosi, Olufemi Olagundoye
Population Medicine
Afolabi Oyapero, Olubukola Olatosi, Olufemi Olagundoye
Population Medicine
2.
Novel tetrahydrocurcumin integrated mucoadhesive nanocomposite κ-carrageenan/xanthan gum sponges: a strategy for effective local treatment of oral cancerous and precancerous lesions
Shimaa Elbanna, Heba Ebada, Ossama Abdallah, Marwa Essawy, Hend Abdelhamid, Hebatallah Barakat
Drug Delivery
Shimaa Elbanna, Heba Ebada, Ossama Abdallah, Marwa Essawy, Hend Abdelhamid, Hebatallah Barakat
Drug Delivery
3.
The global prevalence of oral leukoplakia: a systematic review and meta-analysis from 1996 to 2022
Chang Zhang, Bingjie Li, Xiamei Zeng, XiaoSheng Hu, Hong Hua
BMC Oral Health
Chang Zhang, Bingjie Li, Xiamei Zeng, XiaoSheng Hu, Hong Hua
BMC Oral Health
4.
Prevalence and Malignant Transformation Rate of Oral Erythroplakia Worldwide - A Systematic Review
Kavita Ramesh Wadde, Priyanka Prakash Gajare, Sanpreet Singh Sachdev, Hitesh Rajendra Singhavi
Annals of Maxillofacial Surgery
Kavita Ramesh Wadde, Priyanka Prakash Gajare, Sanpreet Singh Sachdev, Hitesh Rajendra Singhavi
Annals of Maxillofacial Surgery
5.
ASSOCIATION BETWEEN NON-HEALING PRECANCEROUS ORAL LESIONS AND ULCERS WITH TOBACCO SMOKING: A POPULATION-BASED STUDY
Olawale Olatunbosun Adamson, Olufemi Erinoso, Oluremi Oluwakuyide, Abiodun Amao, Olajumoke Effiom, Olalekan Micah Gbotolorun
Oral Oncology Reports
Olawale Olatunbosun Adamson, Olufemi Erinoso, Oluremi Oluwakuyide, Abiodun Amao, Olajumoke Effiom, Olalekan Micah Gbotolorun
Oral Oncology Reports
6.
Self-perceived halitosis and associated factors among university students in Dhaka, Bangladesh
Annesha Dey, Md. Abdullah Saeed Khan, Fahima Nasrin Eva, Tariful Islam, Mohammad Delwer Hossain Hawlader
BMC Oral Health
Annesha Dey, Md. Abdullah Saeed Khan, Fahima Nasrin Eva, Tariful Islam, Mohammad Delwer Hossain Hawlader
BMC Oral Health
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.