INTRODUCTION
One of this millennium’s greatest global health challenges may be attributable to the novel Coronavirus SARS-CoV-2 that causes the COVID-19 infection1. Worldwide, a total of 327 million COVID-19 cases and 5.6 million COVID-19-related deaths have been reported2. Since its discovery in Wuhan Municipality in Hubei Province, China, in December 2019, SARS-CoV-2 has spread rapidly to all continents of the world. Globally, there were more cases reported in the first 5 months of 2021 than in the whole of 20203. The European Union was leading with the highest number of confirmed cases (89.7 million), followed by Asia (85.1 million), North America (67.5 million), South America (40.0 million), African Union (9.9 million), and Oceania (709148)2. Unfortunately, as case numbers continue to rise, more transmissible and dangerous variants are emerging, threatening recovery, and leading to ongoing economic and social disruption, and even more deaths3.
The consequences of the COVID-19 pandemic have been devastating and debilitating, especially in the HICs of the world, which appear to be the epicenter of the disease. It has contributed to the current decrease in global life expectancy (GLE) and average global years of life lost (GYLL) of 16 years4. For instance, the United States’ life expectancy dropped by one point from 78.8 years in 2019 to 77.8 years in the first half of 2020 due to COVID-19-related deaths4,5. A total of 21 million years of life have been lost due to COVID-19 in 81 countries since its emergence in December 20196. The AU shares in this loss as it depends mainly on HICs for survival. It is estimated that 20 million people from the African continent lost their jobs during the COVID-19 pandemic, and the consequences have contributed to increasing poverty, famine, social unrest, and violence7.
The first case of COVID-19 in the African continent was reported in Egypt on 14 February 2020, while Nigeria, which happened to be the first country affected in Sub-Saharan Africa, recorded the first incidence on 27 February 20208. Before the arrival of early cases, control measures were put in place in some AUMCs by their respective national emergency operation centers. These measures included social distancing, personal hygiene, face mask mandate, isolation (quarantine), total lockdown, travel restrictions, and breaking other chains of transmission, including restricting the sales of wild animals for food9.
Africa appears to be the continent with the least reported cases of COVID-19 after Oceania. This feeds a narrative that AUMCs are not adversely impacted by the COVID-19 pandemic when compared to other continents of the world and poses an epidemiologic dilemma. However, the true picture of COVID-19’s impact in Africa is not understood due to inadequate testing in most AUMCs. While a HIC such as the USA had recorded 86.6% testing capacity for COVID-19, the African country with the highest testing capacity was South Africa, with only 13% as of 27 January 202110. In Nigeria, less than 1% of the population has been tested for COVID-19 based on 1.5 million COVID-19 tests conducted during the same period10,11.
There are favorable and unfavorable factors that could possibly demystify the epidemiological dilemma of the COVID-19 hypothesis in Africa. The unfavorable factors are those factors that refute the current reported cases of COVID-19 in the African continent. They are factors occasioned by leadership failure. These factors include weak public health institutions, poor diagnosis/testing capacity, poor health financing, inadequate essential medical supplies, vulnerable populations, and poverty.
Inadequate testing capacity is responsible for the poor contribution of the AU to the global genomic data pool of COVID-19, a condition essential for genomic vaccine production12. As a result of this deficiency, the African continent is a ‘data dark spot’ as it contributed only 90 out of 7700 genome sequences for SARS-CoV-2 pooled from the global community12,13. Also, the African population is a potentially high-risk population for the COVID-19 pandemic due to the increased vulnerability of the people caused by the unhealthy social environment where they are born, grow, live, work, and age14. The social determinants of health of most AUMCs are poor; hence, more African countries have increased capacities to import diseases and low capacities to resist infectious diseases15.
The favorable factors supported the epidemiological picture in 2020 of COVID-19 in the AU. First among these factors is the age structure of the African population. The African continent does not have a much vulnerable age population to COVID-19. The AU is the youngest continent globally, with a median population age of 20 years. The elderly population (>65 years) accounts for only 4% of the African population16. The reverse is in the Asian and European continents, where the elderly population accounts for 37% and 29%, respectively16. It is presumed that since the impact of COVID-19 is more on the elderly population, the African continent is spared from its ravaging menace compared to other continents17.
Secondly, the marginal improvement in the electronic medical record (EMR) system for infectious diseases over the past few years, attributable to previous experiences with outbreaks of viral hemorrhagic diseases (Ebola and Lassa fever), may have improved awareness of health protection (i.e. detection, prevention, and control)14,18. The ERP unit of Africa CDC, in collaboration with the African Task Force for Coronavirus (AFCOR), the World Bank, and other donor agencies, is saddled with the responsibility of regulating COVID-19 preparedness in the AU using six identified thematic approaches of public health protection from COVID-19 infection. The themes include laboratory diagnosis/sub-typing, surveillance by screening at entry and exit of borders, infection prevention and control (IPC) in healthcare facilities, clinical management of people living with COVID-19, risk communication, and supply-chain/stockpiles. These thematic approaches are changing the landscape of the COVID-19 disease trajectory in the AU, with laboratory testing leading the breakthrough18-20.
There is a paucity of data on the comprehensive analysis of the distribution patterns of COVID-19 infection in Africa using epidemiological measures. The availability of these estimates will allow for a better understanding of the trends and variations in COVID-19 infections across the regions and the AUMCs, guide intervention planning and operational responses, ensure the mitigation of the impact of COVID-19 pandemic in the continent, and provide an evidence base which may be useful in preparedness actions for future respiratory pandemics. Therefore, this study aimed to assess the distribution patterns of COVID-19 infection and the associated epidemiological measures across the five geographical regions of Africa and the 53 AUMCs.
METHODS
Study population
The African continent constitutes the study population with a size of 1.394271 billion21. The Western region, which is made up of 15 countries, represents the most populated region with a total population size of 391.965 million (mean=26.131 million). This is followed by the Eastern region, made up of 14 countries with a population of 383.796 million (mean=27.41 million), the Central region, made up of 7 countries with a population of 233.513 million (mean=33.359 million), and the Southern region comprising 10 countries and a population of 180.420 million (mean=18.042 million). The Northern region, comprising 7 countries, has a total population of 155.603 million (mean=29.299 million)21.
Data source
The COVID-19 infection data used for this study were obtained from Africa CDC website (www.africacdc.org) from February 2020 to January 202111. The Africa CDC is a health organization that partners with Africa’s public health institutions to strengthen their capacities and capabilities for disease detection and emergency responses, using datadriven interventions. The Africa CDC operates in six strategic areas, viz. division of disease control and prevention, ERP, laboratory systems networks, national public health institutes and research, public health information systems, and surveillance and disease intelligence. The study data comprised accumulated daily cases of COVID-19 infection from 53 AUMCs within the major geographical regions reported to the Africa CDC. These data covered the five major geographical regions: Northern, Central, Western, Eastern, and Southern. The variables identified in the data included the country’s name, population, geographical region, number of reported cases of COVID-19 infection, number of deaths, active cases, and recoveries. The following epidemiological measures were calculated based on the data obtained, viz. MMRs, CFR, and case ratios22. The COVID-19 testing data were obtained from Our World in Data (https://ourworldindata.org/grapher/full-list-total-tests-for-covid-19)23. Our World in Data collates information from official sources and testing data were available only for 20 countries. Supplementary file Table 1 presents the COVID-19 testing in AUMCs and regions based on available data covering the study period23.
Table 1
Epidemiological measures of COVID-19 infection across geographical regions of the African Union
| Measures | Overall (AU) (N=53) | Geographical region | p | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Central (N=7) | Eastern (N=14) | Northern (N=7) | Southern (N=10) | Western (N=15) | |||||
| Total | Mean | 95% CI | Mean | Mean | Mean | Mean | Mean | ||
| Reported cases (RC) | 3196589 | 60313 | 8102–112525 | 9978 | 24348 | 144958 | 149314 | 185537 | 0.2578 |
| Recoveries (R) | 2582372 | 48724 | 5669–91778 | 4854 | 19021 | 121372 | 119216 | 16022 | 0.2645 |
| Active cases (AC) | 536784 | 10128 | 1880–18375 | 4933 | 4873 | 19761 | 26156 | 2275 | 0.2640 |
| Deaths | 77486 | 1462 | 29–2895 | 191 | 455 | 3824 | 3942 | 240 | 0.2428 |
| R/RC ratio | - | 0.767 | 0.713–0.822 | 0.694 | 0.726 | 0.805 | 0.679 | 0.880 | 0.0617 |
| AC/RC ratio | - | 0.211 | 0.156–0.265 | 0.287a | 0.254a | 0.153ab | 0.303a | 0.099b | 0.0493* |
| Morbidity rate (per 105 population) | 17359 | 327.524 | 178–477 | 94.585bc | 157.741c | 725.844a | 597.307ab | 228.956bc | 0.0449* |
| Mortality rate (per 105 population) | 315.933 | 5.961 | 2.726–9.196 | 1.502bc | 1.835c | 16.796a | 12.048ab | 2.779c | 0.0092** |
| Case-fatality rate (CFR) (%) | - | 2.214 | 1.702–2.727 | 1.825 | 1.966 | 4.128 | 1.829 | 1.991 | 0.0643 |
| Population (million) | 1394 | 26.307 | 16.247–36.368 | 33.359 | 27.414 | 29.229 | 18.042 | 26.131 | 0.9397 |
Statistical analysis
Data obtained were analyzed using both descriptive and inferential statistics. In addition, graphical representations were used to assess the distributional patterns of the epidemiological measures of interest across the AUMCs and regions. A two-tailed test was applied for all statistical tests, and a p<0.05 was used for declaring statistical significance. Data management and statistical analysis were conducted using SAS JMP Statistical DiscoveryTM Software version 14.3 (SAS Institute, Cary, North Carolina, USA)24.
RESULTS
General characteristics
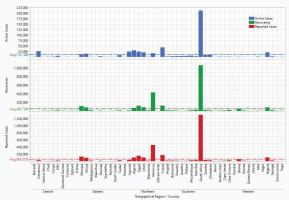
A total of 3.2 million SARS-CoV-2 seropositive cases was reported during the period under review, out of which 77486 died, 536784 were active cases, and 2.6 million recovered (Table 1). The mean number of reported cases of COVID-19 in the AU was 60313. Southern Africa had the highest number of reported cases (149000), while Central Africa recorded the least (9980). About nine countries (South Africa, Morocco, Tunisia, Egypt, Ethiopia, Libya, Nigeria, Algeria, and Kenya) had reported cases greater than the mean reported cases of COVID-19 infection in the AU (Figure 1). However, there was no statistically significant difference (p=0.2578) in mean reported cases across the geographical regions of the AU (Table 1). Although COVID-19 testing data was not available from Africa CDC, data obtained elsewhere (Our World in Data), and based on reporting countries, a total of 83828061 tests were performed between February 2020 through January 2021. Of this number, the majority of the tests (≥70%) were performed in the Southern (48.9%, n=41.011 million) and Northern (21.93%, n=18.380 million) regions (Supplementary file Table 1).
Recoveries in the AU
The mean number of recoveries from COVID-19 in the AU was 48724. Northern Africa recorded the highest mean recoveries (n=121372), while Central Africa had the least (n=4854) in descending order of magnitude of Northern >Southern >Eastern >Western >Central. A total of nine countries had recoveries greater than the mean recoveries of COVID-19 in the AU. No statistical difference was recorded in mean recoveries across the geographical regions (p=0.2645) (Table 1). The patterns of recoveries among the AU member nations are shown in Figure 1.
AC in the AU
A mean AC of 10128 was recorded in the AU. Southern Africa had the highest AC (n=26156), while Western Africa recorded the least AC (n=2275) (Table 1). In descending order of magnitude, the Southern >Northern >Central >Eastern >Western. Eleven countries (South Africa, Tunisia, Algeria, Cameroun, Uganda, Egypt, Nigeria, Libya, Morocco, Kenya, and Ethiopia) recorded AC greater than the mean AC reported in the AU (Figure 1). In all the regions, the mean AC was less than the mean R, except in Central Africa where the mean AC was greater than the mean number of recoveries. There were no statistically significant differences in the AC across the geographical regions of the AU (p=0.264).
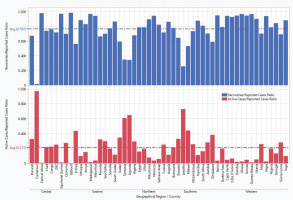
R/RC and AC/RC ratios
As expected, we noted an inverse relationship between the R/RC and AC/RC ratios such that as the R/RC ratio rises, the AC/RC ratio decreases. The AU’s mean R/RC and AC/RC ratios were 0.767 and 0.211, respectively (Figure 2). There was a significant difference (p=0.0493) in the AC/RC ratios across the geographical regions of the AU (Table 1). Thirty (56.6%) member countries had an R/RC ratio above the mean of 0.767. Twenty countries (37.7%; 5 each from Southern, Central, and Eastern regions; 3 and 2 from Northern and Western regions, respectively) recorded AC/RC ratios above the mean for the AU. The Western region had the highest R/RC (0.880) and lowest AC/RC (0.099) ratios, while the Southern region recorded the highest AC/RC (0.301) and lowest R/RC (0.679) ratios. However, there was no statistically significant difference (p=0.0617) in the mean R/RC ratios across the geographical regions of the AU. The distribution patterns of the case ratios (AC/RC and R/RC) of COVID-19 in the AUMCs by geographical region are shown in Figure 2.
COVID-related deaths
A total of 77690 COVID-related deaths was recorded in the AU during the period under review (mean=1462). The Southern region had the highest mean death toll of 3942, while the Central region recorded the lowest number of deaths (mean=191). The top-nine countries (Figure 3) with the high number of COVID-related deaths in descending order were South Africa (n=36467), Egypt (n=8473), Morocco (n=7888), Tunisia (n=5528), Algeria (n=2827), Ethiopia (n=2023), Kenya (n=1726), Libya (n=1651) and Sudan (n=1576). Nonetheless, there was no statistically significant difference in the number of COVID-related deaths across the geographical regions of the African Union (p=0.243) (Table 1).
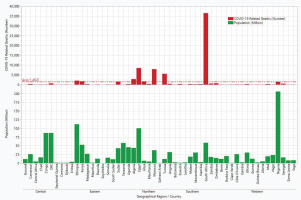
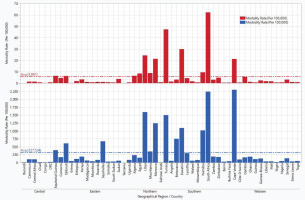
Morbidity and mortality rates
The mean MMRs of COVID-19 in the AUMCs were 327.52 and 5.961 per 100000 people. We noted significant variations in morbidity (p=0.0449) and mortality (p=0.0092) rates of COVID-19 across the geographical regions of the AU (Table 1). The Northern region recorded the highest MMR of 725.84 and 16.796 per 100000 people, while Central Africa had the lowest MMR values of 94.58 and 1.502, respectively. The MMR followed the same descending order of magnitude across the regions of the AU with Northern >Southern >Western >Eastern >Central. However, three regions (Western, Eastern, and Central) recorded MMR below the overall mean rates for the AU. The top nine leading countries in the AU with higher morbidity rates for COVID-19 infection in descending order were Cape Verde, South Africa, Libya, Tunisia, Morocco, Eswatini, Botswana, Seychelles, and Djibouti. Similarly, the top six leading countries with higher COVID-19 mortality rates in descending order were South Africa, Tunisia, Eswatini, Libya, Cape Verde, and Morocco. Burundi had the least morbidity rate of 0.017 per 105 population. The distribution of morbidity and mortality rates of COVID-19 in the AUMCs by geographical region is presented in Figure 4.
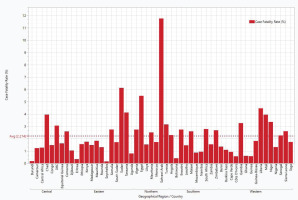
CFR of COVID-19 in the AU
The overall mean CFR of 2.21% was obtained in the AU, with the highest and lowest CFR recorded in the Northern (4.12%) and Central (1.82%) regions, respectively (Table 1). Although not statistically significant (p=0.0643), numerical differences were noted across regions and countries. For instance, 22 countries (22/53; 41.51%) recorded CFR above the mean value of 2.21%. Sahrawi Arab recorded the highest CFR (11.76%) among the member countries of the AU, while Seychelles had the lowest CFR (0.15%). The CFR of COVID-19 in AUMCs within the five geographical regions is presented in Figure 5.
DISCUSSION
The COVID-19 pandemic introduced a new world order by ironically eliciting different narratives and unhealthy speculations on the wealthier nations of the world with respect to reported cases of the COVID-19 infection between 2020 and January 202125. Our study recorded a total of 3.2 million reported cases of COVID-19 in a population of approximately 1.4 billion people with a mean CFR of 2.21%. This CFR was greater than that of the global average (2.15%), New Zealand (1.1), and the USA (1.7)26. This shows that although the AU appears to have the least RC of COVID-19 compared to other continents, the COVID-19-related death rate is rising in Africa27. Unfortunately, the reported cases do not reflect the impact of COVID-19 on the population of the AU. This could be attributable to the poor testing capacities of many AU countries. Inaccurate reporting of COVID-19 deaths in Africa may result in a false estimation of community vulnerability to COVID-1928. The COVID-19 trending patterns in AUMCs will be better appreciated by implementing the COVID-19 screening policy as a public health safety measure. The study by Ilesanmi and Afolabi29 in AUMCs showed that strategic implementation of combined public health safety measures could either increase or reduce COVID-19 reported cases depending on the stringency levels of implementation. A high stringency level of implementation of the COVID-19 screening test across the AUMCs and regions will help to demystify the COVID-19 epidemiologic dilemma in the regions. According to available statistics, 1 in 6 South African citizens tested COVID-19 seropositive while 1 in 12 Nigerians was seropositive10. The latter was comparable to that of the USA, where 1 in 11 people tested positive to COVID-1910,11. This result shows that South Africa, an AU country, was worse hit than the USA. A true picture of the impact of COVID-19 in the AU would have been revealed if more robust tests had been conducted in the AUMCs.
The Southern and Northern regions of Africa recorded mean RCs double that of the AU, while the Eastern, Western, and Central regions were 2.5, 3.0, and 6.0 times lower. This shows that the Southern and Northern African regions are 12, 6, and 5 times ahead of the AU’s Central, Western, and Eastern regions, respectively, regarding COVID-19 testing. South Africa has the best testing statistics and medical infrastructure for capacity building in the continent. These factors, together with the virulent new variant of COVID-19 (SARS-CoV-2-B.1.351, also known as the South African variant of COVID-19) and probably the long government response time, contributed to the high RC, AC, and D in the country30-32. Testing remains the most sought health tool for responding to and monitoring the virus spread. Consequently, poor testing and inadequate availability of vaccines in the AU can create the perfect conditions for more virulent and deadly strains of COVID-19 to surface. The emergence of COVID-19 variants can undermine the efficacy of existing vaccines and treatments and will inevitably spread across the world, thus putting at risk even those countries that have made the most progress in vaccinating their population33. It has been estimated that the LMIC needs at least 900 million tests in 20213. However, with the recent global partnership with numerous international organizations, including the Africa CDC, to provide over 63 million COVID-19 molecular and rapid diagnostic tests (Ag RDTs) kits and accelerate equitable deployment of vaccines to LMIC34, the AU has an opportunity to scale-up the testing, tracing, and treatment of COVID-19 cases promptly at the point of care, particularly in areas with under-resourced health systems.
Despite the 1.4 billion population of Africa, it still has the least COVID-19 cases and testing numbers comparatively. Some researchers have attributed those to poor health systems, limited testing capacity, and poor reporting systems35,36, while others credited it to early mitigatory responses, enhanced by leveraging existing infection control systems, government political will37, and the generally low risk of virus importation from COVID-19 hotspots38.
Furthermore, our study showed that those who recovered from COVID-19 were more in the Western region than in other AU regions. The probable reasons may be related to immunity and the youthful population that make up a large proportion of the Western region of the AU13. On the other hand, there was a statistically significant difference in AC/RC ratio across the AU regions. The Southern region led with a high AC/RC ratio, probably due to the highly contagious mutant strain of COVID-19 and the associated heavy disease burden on healthcare facilities30. As of 28 January 2021, it was reported that 1 in 2 new RC of COVID-19 was from South Africa21. There are speculations that one of the newly manufactured vaccines against SARS-CoV-2 (i.e. AstraZeneca/Oxford vaccine) does not provide adequate protection against this variant of COVID-1932. As a result of this deficiency, the use of this vaccine was stopped in South Africa34.
The Northern and Southern regions bear a higher COVID-19 disease burden than Central, Eastern, and Western Africa combined. In contrast, Cape Verde (a small island in West Africa) and South Africa are the top two countries with the highest morbidity rates of COVID-19 in the AU. Both countries share one thing in common: they are tourist countries. As tourist nations, both countries have increased capacities to import diseases (high SPAR score) and more vulnerability to diseases (low IDVI)15.
Generally, the COVID-related deaths across the AU were, however, not proportionally related to the population size of the member countries. For example, South Africa, with a population size of 57 million, recorded the highest number of deaths, while Nigeria, Africa’s most populous Black nation with a population size of 206 million, was not among the top nine countries with the highest COVID-related death.
Strengths and limitations
The data used for this study were obtained from the Africa CDC and Our World in Data websites, and so, did not have needed variables for the assessment of all the epidemiological measures of interest for monitoring and evaluation of the impact of the COVID-19 pandemic in the AU member nations. For instance, the testing data were only available for selected countries (n=20) that make up the five geographical regions of AU at the time of this study and did not distinguish between positive and negative test results. Thus, the data presented may not be representative of the AU and the regions in terms of the actual number of COVID-19 tests performed during the period under review. Undercounting or ignoring cases of COVID-19 has been reported to be a major setback in predicting a true picture of the COVID-19 pandemic’s impact in Africa39. The large variability in case numbers (too large or small) obtained across AUMCs and regions, with resultant effects on the epidemiological measures determined, led to nonsignificant results in some cases despite huge numerical differences. Accordingly, caution should be exercised in the interpretation of the results, with consideration given to the clinical relevance and implication of the findings, whether the results are statistically significant or not40. Nevertheless, these limitations may provide opportunities to inform future research. We must leverage the strengths of this study which include the estimation of epidemiological measures for all the AU member nations and across the regions. These measures have given insight into the distribution patterns of COVID-19 in Africa, hence providing the basis for comparison among the AUMCs, and with HICs of the world. The findings of this study, therefore, have the potential to demystify the epidemiological dilemma of the COVID-19 pandemic in the AU and offer the opportunity for the implementation of an effective and appropriate intervention to curb the chains of transmission of COVID-19.
CONCLUSIONS
Although testing is a critical cornerstone of the COVID-19 response, the poor availability of test types that can be used in different settings and situations in the AU remains a constraint. The COVID-19 testing capacities of the Northern and Southern regions of the AU are more robust compared to their Central, Eastern, and Western counterparts, as evidenced by the high number of COVID-19 tests and the confirmed cases reported in those regions. This results in high MMRs of COVID-19 and present the Northern and Southern regions as worse hit by the pandemic. The current low testing capacity in the Central, Western, and Eastern regions of Africa, coupled with the poor reporting systems, do not provide strong evidence for the assessment of the impact of COVID-19 in some parts of AU. Therefore, the advocacy should be more on scaling-up case ascertainment of COVID-19 through testing and sub-typing in these regions, in addition to providing insight into potential emergency preparedness and response measures in the light of future respiratory epidemics. By so doing, the AU will become much more relevant in the global genomic data pool of COVID-19.